Fat is a strategic product , a kind of “stew warehouse” in the body. We got it as a result of thousands of years of evolution, because our ancestors had serious problems with nutrition, and adipose tissue reliably saved us from hunger. It is more difficult to break down than other nutrients, so getting rid of its excess is very difficult.
For example, let’s take a girl weighing 60 kg of normal build. Such a girl has about 15 kg of fatty tissue in her body, that is, 110 thousand kilocalories. Such reserves are enough to survive for 2 months before irreversible consequences begin.
In addition, fats participate in the functioning of the endocrine system, performing a transport function. Extreme values can lead to serious problems with the thyroid gland, menstrual cycle and liver function.
Another important function of fat is thermal insulation. In other words, fat keeps us warm in cold times. This function is mainly performed by subcutaneous fat.
Remember walruses - their fat layer will be the envy of any resident of the Arctic.
There is also visceral fat, which, on the one hand, performs a thermoregulatory function, and on the other, a supporting one. It envelops the internal organs (heart, stomach, intestines, etc.) to keep them in the “right” places and protect them from damage.
With a lack of adipose tissue, problems are observed with thermoregulation and the supporting function of internal organs, with the absorption of fat-soluble vitamins (A, D, E, K), as well as rapid aging of the skin, dry hair and nails. In addition, if there is a lack of fat, survival mode is activated when the body simply will not meet your daily demands. With excess fat, body weight increases, which brings inconvenience, internal organs are literally compressed and cannot function fully, and there are problems with oily skin.
And most importantly: with both a deficiency and an excess of adipose tissue, problems begin with hormones, the functioning of all body systems, cycle disruptions and sudden mood swings.
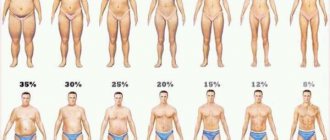
That is why it is important and necessary to at least visually represent your fat percentage and adjust it if necessary.
How to measure?
Stand up straight, straighten your back. Grab the fold of skin and fat just below the navel horizontally - thumb on top, index finger on bottom. Place the ruler horizontally, resting its end on the stomach, and measure the thickness of the fold in millimeters. Then find the resulting value in the table below based on your age. The content of adipose tissue in the body of women (in percent)
| Subcutaneous fat fold, mm | 18-29 years old | 30-39 years old | 40-49 years old | 50 or more years |
| 15 | 10,5 | — | — | — |
| 20 | 14,1 | 17 | 19,8 | 21,4 |
| 25 | 16,8 | 19,4 | 22,2 | 24 |
| 30 | 19,5 | 21,8 | 24,5 | 26,6 |
| 35 | 21,5 | 23,7 | 26,4 | 28,5 |
| 40 | 23,4 | 25,5 | 26,2 | 30,3 |
| 45 | 25 | 26,9 | 29,6 | 31,9 |
| 50 | 26,5 | 28,2 | 31 | 33,4 |
| 55 | 27,8 | 29,4 | 32,1 | 34,6 |
| 60 | 29,1 | 30,6 | 33,2 | 35,7 |
| 65 | 30,2 | 31,6 | 34,1 | 36,7 |
| 70 | 31,2 | 32,5 | 35 | 37,7 |
| 75 | 32,2 | 33,4 | 35,9 | 38,7 |
| 80 | 33,1 | 34,3 | 36,7 | 39,6 |
| 85 | 34 | 35,1 | 37,5 | 40,4 |
| 90 | 34,6 | 35,8 | 38,1 | 41,2 |
| 95 | 35,6 | 36,5 | 39 | 41,9 |
| 100 | 36,4 | 37,2 | 39,7 | 42,6 |
| 105 | 37,1 | 37,9 | 40,4 | 43,3 |
| 110 | 37,8 | 38,6 | 41 | 43,9 |
| 115 | 38,4 | 39,1 | 41,5 | 44,5 |
| 120 | 39 | 39,6 | 42 | 45,1 |
| 125 | 39,6 | 40,1 | 42,5 | 45,7 |
| 130 | 40,2 | 40,6 | 43 | 46,2 |
| 135 | 40,8 | 41,1 | 43,5 | 46,7 |
| 140 | 41,3 | 41,6 | 44 | 47,2 |
| 145 | 41,8 | 42,1 | 44,5 | 47,7 |
| 150 | 42,3 | 42,6 | 45 | 48,2 |
| 155 | 42,8 | 43,1 | 45,4 | 48,7 |
| 160 | 43,3 | 43,6 | 45,8 | 49,2 |
| 165 | 43,7 | 44 | 46,2 | 49,6 |
| 170 | 44,1 | 44,4 | 46,6 | 50 |
| 175 | 44,4 | 44,8 | 47 | 50,4 |
| 180 | 44,7 | 45,2 | 47,4 | 50,8 |
| 185 | 45 | 45,6 | 47,8 | 51,2 |
| 190 | 45,3 | 45,9 | 48,2 | 51,6 |
| 195 | 45,5 | 46,2 | 48,5 | 52 |
| 200 | 45,5 | 46,5 | 48,8 | 52,4 |
| 205 | 45,8 | 46,8 | 49,1 | 52,7 |
| 210 | 46 | 47,1 | 49,4 | 53 |
Content of adipose tissue in the body of men (in percent)
| Subcutaneous fat fold, mm | 18-29 years old | 30-39 years old | 40-49 years old | 50 or more years |
| 15 | 4,8 | — | — | — |
| 20 | 8,1 | 12,2 | 12,2 | 12,6 |
| 25 | 10,5 | 14,2 | 15 | 15,6 |
| 30 | 12,9 | 16,2 | 17,7 | 18,6 |
| 35 | 14,7 | 17,7 | 19,6 | 20,8 |
| 40 | 16,4 | 19,2 | 21,4 | 22,9 |
| 45 | 17,7 | 20,4 | 23 | 24,7 |
| 50 | 19 | 21,5 | 24,6 | 26,5 |
| 55 | 20,1 | 22,5 | 25,9 | 27,9 |
| 60 | 21,2 | 23,5 | 27,1 | 29,2 |
| 65 | 22,2 | 24,3 | 28,2 | 30,4 |
| 70 | 23,1 | 25,1 | 29,3 | 31,6 |
| 75 | 24 | 25,9 | 30,3 | 32,7 |
| 80 | 24,8 | 26,6 | 31,2 | 33,8 |
| 85 | 25,5 | 27,2 | 32,1 | 34,8 |
| 90 | 26,2 | 27,8 | 33 | 35,8 |
| 95 | 26,9 | 28,4 | 33,7 | 36,6 |
| 100 | 27,6 | 29 | 34,4 | 37,4 |
| 105 | 28,2 | 29,6 | 35,1 | 38,2 |
| 110 | 28,8 | 30,1 | 35,8 | 39 |
| 115 | 29,4 | 30,6 | 36,4 | 39,7 |
| 120 | 30 | 31,1 | 37 | 40,4 |
| 125 | 30,5 | 31,5 | 37,6 | 41,1 |
| 130 | 31 | 31,9 | 38,2 | 41,8 |
| 135 | 31,5 | 32,3 | 38,7 | 42,4 |
| 140 | 32 | 32,7 | 39,2 | 43 |
| 145 | 32,5 | 33,1 | 39,7 | 43,6 |
| 150 | 32,9 | 33,5 | 40,2 | 44,1 |
| 155 | 33,3 | 33,9 | 40,7 | 44,6 |
| 160 | 33,7 | 34,3 | 41,2 | 45,1 |
| 165 | 33,7 | 34,6 | 41,6 | 45,6 |
| 170 | 34,5 | 34,8 | 42 | 46,1 |
| 175 | 34,9 | 35 | 42,4 | 46,5 |
| 180 | 35 | 35,2 | 42,8 | 46,9 |
| 185 | 35,6 | 35,4 | 43 | 47,3 |
| 190 | 35,9 | 35,6 | 43,3 | 47,7 |
Hips and buttocks
Too massive hips are the scourge of many women. Fat is most often deposited in this part of the body among lovers of cakes, chocolate and other sweets, as well as coffee and fried foods. And it is sometimes very difficult to part with it, because women lose weight from top to bottom - first the face, then the upper body and arms, then the stomach, and at the very end - the legs and buttocks.
Among men, this problem is not so common, and the most common cause of fat legs is sugary carbonated drinks. Moreover, it is easier for them to get rid of fat thighs because their fat tissue has a different structure.
The illusion of satiety: a list of foods that make you want to eat even more
When is the method useful?
Typically, healthy weight limits are calculated using the body mass index
(BMI) formula.
But the resulting value does not always reflect the real picture. An increased BMI can be observed in people with developed muscles, while a normal BMI can be observed in an unathletic person with a fragile physique and decent fat reserves. To more accurately determine your condition, it is better to evaluate two indicators at once
- BMI and body fat percentage.
For example, if, with a decrease in BMI, the percentage of fat remains unchanged, weight loss occurs due to a decrease in muscle mass, which can be called exhaustion of the body. If BMI increases, a change in the percentage of fat will show whether the weight is increasing - muscle mass is growing, or fat reserves are being deposited. According to Korochkin, this method of calculation is suitable for those who regularly train to lose weight. In this situation, it is not the exact knowledge of weight, BMI and body fat percentage that is important, but the change in these values over time
. “Even if there is an error in the table or your measurements,” notes Korochkin, “the dynamics of changes in values will show whether you are moving in the right direction.”
Look beyond the weight scale
The scale can't tell you exactly how much fat you have in your body, but these indicators can:
- Wardrobe: clothes have become big? Are you able to wear more and more things from your youth?
- Sets and Reps in the Gym: Has Performance Improved? Can you exercise longer, lift heavier weights, or perform exercises without the same effort?
- Daily tasks: Do you find it easier to carry bags or clear snow in winter?
- Energy levels: Do you feel more fit and less tired when you wake up?
- Reflection: how do you look in the mirror - flabby or toned and sexy?
How to estimate your body fat percentage
Relative content of adipose tissue in the body of women (in percent)
| Characteristic | Age, years | ||||
| 18-29 | 30-39 | 40-49 | 50-59 | >60 | |
| Very low | |||||
| Low | 16-19 | 17-20 | 18-21 | 19-22 | 20-23 |
| Optimal | 20-28 | 21-29 | 22-30 | 23-31 | 24-32 |
| Moderate high | 29-31 | 30-32 | 31-33 | 32-33 | 33-35 |
How to lose weight through sports?
Basic rules of training, diet and useful links in the material for those who want to learn how to lose weight correctly and reliably.
Relative content of adipose tissue in the body of men (in percent)
| Characteristic | Age, years | ||||
| 18-29 | 30-39 | 40-49 | 50-59 | >60 | |
| Very low | |||||
| Low | 11-13 | 12-14 | 14-16 | 15-17 | 16-18 |
| Optimal | 14-20 | 15-21 | 17-23 | 18-24 | 19-25 |
| Moderate high | 21-23 | 22-24 | 22-26 | 25-27 | 26-28 |
Sensational news about brown fat
Two studies in an English medical journal about a special form of thermogenically active fat tissue that releases excessive amounts of energy when processed have unexpectedly attracted media attention. One headline even read: "Brown Fat: The Fat That Will Help You Lose Weight?"
"Brown or brown fat generally doesn't matter," says Fabio Comana, an exercise physiologist at the American Council on Exercise. “Thousands of years ago, it helped keep us warm during the cold months.” But these days we don't have to worry about cold weather - we have clothes, houses and heaters, so it's mostly hype.
If there is too little fat?
A reduced body fat content is not a reason for pride, but a reason for reviewing your diet.
Lack of adipose tissue in the body disrupts the functioning of the endocrine system. In this case, women may stop menstruating and experience early signs of osteoporosis, a disease in which bones lose calcium and become very fragile. In addition, if the fat layer in the lower back and hips completely disappears, the kidneys and organs of the reproductive system are deprived of protection from the cold. When hypothermia occurs, a woman runs the risk of developing inflammatory processes in the pelvic organs. Myths about losing weight
Are there products to burn fat in specific areas? Is it possible to lose weight quickly and effectively? What do the scales show before and after training? Let's talk.
What is the best way to find out how much body fat you have?
Examples of ways to measure fat:
Caliper
Cost: from 900 to 24,000 rubles
Accuracy: error rate ±3%; basically measures fat under the skin
Availability: most fitness clubs
Appliances for home use
Cost: from 1,200 to 18,000 rubles for a machine that determines body fat using the electrical resistance method
Accuracy: error rate ±3%
Availability: Can be purchased online
Hydrostatic test (underwater)
Cost: from 900 to 3000 rubles per test
Accuracy: error rate ± 1.5%
Availability: Typically conducted at research institutes and universities
If there is too much fat?
Too much body fat indicates an increased risk of developing cardiovascular diseases and metabolic diseases, such as hypertension and type 2 diabetes. Particularly dangerous for both men and women is the so-called abdominal obesity - the deposition of fat reserves in the waist area. It increases the risk of developing cardiovascular disease by five times. A real cause for alarm appears when the waist circumference in men exceeds 102, and in women - 88 centimeters.
Hands
The average man has more muscle mass in his arms than the average woman, which is why full, shapeless arms stand out so clearly among the fairer sex. In these places, fat is deposited in lovers of sweets, as well as fatty meats and dairy products. In addition, full arms can indicate an excess of insulin or a lack of testosterone (yes, the female body also produces male hormones).
Photo: istockphoto.com
The main male hormone. What to eat to increase testosterone levels
Factors influencing weight gain
Obesity is a complex disease that results from a combination of many different aspects of a person's life that occur over a long period of time. A woman's weight can be affected by:
Genes and family background. Obesity is usually inherited. But there is no specific “fat” gene. There are many genes that can work together to increase your likelihood of gaining weight. The situation in which a woman lives also affects her genes. When the child is a small child, parents control nutrition and physical activity. This family background may influence adult weight.
Metabolism. Metabolic rate (how quickly your body burns calories) can vary for many reasons, and this can affect weight gain and loss. For example, men typically have more muscle and less fat than women, so men's bodies can burn more calories and do so much faster. A woman's metabolism can change throughout her life, for example due to hormonal changes that occur during puberty, pregnancy and menopause.
Age. As you age, your metabolism can slow down. In addition, as women age, they lose muscle. With less muscle to burn calories, the body needs fewer calories.
Mental trauma. Women who experience a traumatic event at any time, are stressed, or have post-traumatic stress disorder (PTSD) may be more likely to gain weight quickly after the traumatic event and develop obesity.
Medicines. Many of the medications women take every day, including medications for mental health problems, sleep disorders and high blood pressure, can cause weight gain or make it difficult to lose.
Sleep disorders. Lack of quality sleep can lead to weight gain. Researchers believe this may be due to poor quality sleep, which can affect levels of hormones that regulate appetite and food choices. Lack of sleep without adequate rest can also affect your physical activity or exercise performance during the day.
Visceral obesity in patients with different body mass indices
Summary . The relationship between body mass index (BMI), visceral adipose tissue, and triglycerides (TG), glucose, and high-density lipoprotein cholesterol (HDL-C) levels was assessed. A total of 150 patients were examined.
In individuals with different degrees of obesity according to BMI, no significant differences were found in the amount of visceral adipose tissue and in the effect on the levels of TG, glucose and HDL-C. An increase in the content of visceral adipose tissue leads to a significant increase in the level of triglycerides and glucose and a decrease in the content of HDL-C. In patients with visceral adipose tissue content less than 10%, the median TG was 1.13 [0.76; 1.46] mmol/l; glucose 5.52 [4.99; 5.71] mmol/l; HDL-C 1.24 [1.06; 1.42] mmol/l. In patients with visceral adipose tissue content of 11% or more, the median TG was 1.585 [1.12; 2.12] mmol/l; glucose 5.97 [5.46; 6.93] mmol/l; HDL-C 1.02 [0.86; 1.31] mmol/l. All differences are highly significant - p < 0.004. The level of visceral adipose tissue of 16% or more is combined with an increase in median TG and glucose above normal values: more than 1.7 mmol/l and 6.5 mmol/l, respectively.
The degree of obesity does not reflect the severity of metabolic disorders, which play an important role as factors in the development of cardiovascular diseases. The accumulation of visceral adipose tissue is clearly associated with increased TG and glucose levels and decreased HDL-C levels. Thus, the existing classification of obesity by degree does not take into account the accumulation of visceral adipose tissue, which has the most adverse effect on metabolic disorders and, accordingly, on the risk of developing CVD.
Over the past 30 years, the prevalence of obesity has doubled in many countries. For example, in the USA, the number of people with excess body weight of 30 kg/m2 or more increased by 35% and 40% among men and women, respectively [1].
In Russia, as of the end of 2016, 23.5 million obese people were registered [2]. In 2013, the Russian Federation ranked 19th among all countries in the world in terms of obesity prevalence, lagging behind Mexico and the United States, which topped the list, by 8% [3].
A more in-depth analysis showed that for individuals with the same body mass index (BMI), the risk of disease and death is not the same [4]. In addition, not all obese individuals have metabolic risk factors (MRFs) for the development of cardiovascular diseases (CVD), which served as the basis for the formation of ideas about the existence of metabolically healthy obesity [5, 6]. The use of computed tomography (CT) and magnetic resonance imaging (MRI) has established that abdominal obesity (AO) in different individuals is combined to varying degrees with the presence of metabolic risk factors for the development of atherosclerosis. These data are now explained by the fact that subcutaneous obesity in the abdominal area has little effect on the risk of developing CVD [7]. It is with the accumulation of visceral adipose tissue, which is localized inside the abdominal cavity, behind the muscles of the anterior abdominal wall, between internal organs and in the retroperitoneal space, that the development of metabolic disorders and CVD is associated [1, 8–9].
Considering that CT and MRI, used in scientific studies, are not available for widespread use in the practical work of a doctor when examining the population and patients, it seems important to evaluate the information content of simple and accessible methods for determining visceral fat and, in particular, the bioimpedance method, based on determining the difference in conducting an electrical signal in fat and muscle tissues [10].
This method has received approval from the Food and Drugs Administration of the United States (FDA) [11].
Material and research methods
The observational study assessed anthropometric parameters of height, weight, BMI, waist circumference, percentage of adipose tissue and, separately, percentage of visceral adipose tissue, as well as the relationship of these parameters with blood lipid profile and glucose levels. Assessing the effect of visceral adipose tissue on cholesterol levels—total and low-density lipoprotein cholesterol (LDL-C)—was complicated by the fact that all patients were on statin therapy at the time of inclusion in the study.
A total of 154 patients who were treated in the Department of Myocardial Diseases and Heart Failure of the National Medical Research Center of Cardiology were examined. Of these, 68 are women and 86 are men. The median age of patients was 63 [55; 69] year.
Height was measured using a metal stadiometer with a movable spring-loaded clamp Rm-1 "Dicoms", the measurement results were expressed in centimeters (cm). Weight, BMI, percentage of total and visceral adipose tissue were measured using an Omron BF-508 body composition monitor, which measures percentage of body fat using the bioelectrical impedance method. The essence of the method is that muscles, blood vessels and bones contain a lot of water, being good conductors of electricity. Adipose tissue has poor electrical conductivity. To determine the amount of fat tissue, the Omron BF-508 device passes an extremely weak electrical current through the body with a frequency of 50 kHz and an intensity of less than 500 μA. When assessing body composition, the device takes into account total electrical resistance, as well as height, weight, age and gender. Waist circumference was measured using a measuring tape at the midpoint of the distance between the lower edge of the ribs and the iliac crest with the patient standing. Pathological values, according to existing recommendations, were considered to be a waist circumference equal to or greater than 102 cm in men and 88 cm in women [12, 13].
The hypothesis of normal distribution of some characteristics, in particular the percentage of visceral fat, was rejected using the Shapiro-Wilk test, as a result of which non-parametric methods of analysis and estimation were subsequently used. In the tables, the obtained values are presented in the form Me [LQ; UQ], where Me is the median, LQ; UQ—interquartile range. The significance of differences in all parameters of quantitative traits was determined using the Mann–Whitney U test. For all types of analysis, differences were considered statistically significant at p < 0.01.
Research results
Of the 154 patients examined, the leading pathology in 93 people was coronary heart disease (CHD), isolated in a smaller percentage of cases (10 people), and in most cases in combination with arterial hypertension (83 people). Arterial hypertension, isolated or in combination with cardiac arrhythmias, was diagnosed in 61 patients.
According to the existing classification of obesity based on BMI, out of 154 patients examined, 13 people had normal weight (BMI ranging from 18.5 to 24.9 kg/m2), 60 people were overweight (BMI ranging from 25.0 to 29 .9 kg/m2), 81 people had obesity: 46 people had 1st degree obesity (BMI 30–34.9 kg/m2), 20 people had 2nd degree obesity (BMI 30–34.9 kg/m2) and in 15 people - degree 3 (BMI ≥ 40 kg/m2).
A significant increase in the content of visceral adipose tissue from normal weight to different degrees of obesity was noted. In patients with excess body weight, the percentage of visceral adipose tissue was significantly higher than in patients with normal weight: 11 [10; 13] vs 7 [7; 9], p = 0.001. In turn, in individuals with grade 1–3 obesity, the percentage of visceral adipose tissue significantly increases compared to individuals with overweight and normal weight (p = 0.001). However, no significant differences in the percentage of visceral adipose tissue were found between individuals with different degrees of obesity (p > 0.1). The data is presented in table. 1 and 2.
The content of total adipose tissue, expressed as a percentage, differed significantly among individuals with different BMIs (p ≤ 0.02).
Further analysis showed that an increase in the content of visceral adipose tissue leads to an increase in the level of triglycerides and glucose and a decrease in the content of high-density lipoproteins. There were no significant differences in the levels of total cholesterol and LDL-C, which may be due to the fact that the patients were on statin therapy for a long time, which significantly affects the above indicators and has little effect on the levels of triglycerides and glucose.
We divided the patients into 4 groups depending on the content of visceral adipose tissue. The 1st group included patients with the least amount of visceral adipose tissue from 0% to 10%, the 2nd group included patients with a level of visceral adipose tissue from 11% to 15%, the 3rd group included patients with a visceral adipose tissue content from 16 % up to 20% and in the 4th - with a level of visceral adipose tissue more than 21%.
A significant increase in the level of triglycerides and glucose was revealed between group 1 and groups 3–4, as well as between group 2 and groups 3–4. Moreover, in groups with a high content of visceral adipose tissue (16% or more), triglycerides and glucose levels go beyond normal values. In terms of reducing the level of high-density lipoprotein cholesterol (HDL-C), significant differences were found between group 1 and groups 3–4. The numerical values of triglycerides, glucose and HDL cholesterol are presented in table. 3.
Significance of differences in triglyceride levels between groups 1 and 3 - p = 0.0000001; between the 1st and 4th groups - p = 0.002.
Significance of differences in glucose levels between groups 1 and 3 - p = 0.0000001; between the 1st and 4th groups - p = 0.0000001.
Significance of differences in HDL-C between groups 1 and 3 - p = 0.015; between the 1st and 4th groups - p = 0.001.
Significance of differences in triglyceride levels between groups 2 and 3 - p = 0.002; between the 2nd and 4th groups - p = 0.005.
Significance of differences in glucose levels between groups 2 and 3 - p = 0.008; between the 2nd and 4th groups - p = 0.008.
For clarity, we made an additional comparison between group 1 with the lowest visceral fat content and the sum of groups 2–4. The results are presented in table. 4.
At the same time, in patients with different BMI values, significant differences were detected in the level of triglycerides between patients with normal weight and obesity of the 1st, 2nd, 3rd degrees (p ≤ 0.01); by glucose level - between patients with normal weight and obesity of the 1st, 2nd degree (p ≤ 0.005) and between patients with overweight and obesity of the 1st degree (p = 0.005). There were no significant differences in the levels of triglycerides, glucose and HDL-C in patients with different degrees of obesity. The numerical values of triglycerides, glucose and HDL cholesterol are presented in table. 5.
Discussion
Based on the results of our study, we were able to establish that an increase in the content of visceral adipose tissue, determined according to the bioimpedance method of research, is combined with a significant increase in the level of triglycerides and glucose, as well as a decrease in the content of HDL-C, which in turn can play a role in the progression of atherosclerosis , since high levels of HDL cholesterol are considered as a factor slowing the progression of atherosclerosis.
At the same time, the increase in the degree of obesity, determined on the basis of BMI, was not associated with a significant increase in the levels of triglycerides and glucose, as well as a decrease in HDL-C. This once again emphasizes the role of visceral adipose tissue in the formation of metabolic disorders. Thus, by now there is a need to revise the classification of obesity taking into account the level of visceral adipose tissue.
Visceral adipose tissue differs significantly from subcutaneous adipose tissue in the type of fat cells (adipocytes), their endocrine function, lipolytic activity, response to insulin and other hormones. Along with its location in close proximity to internal organs, visceral adipose tissue is also characterized by better vascularization and innervation. In visceral adipose tissue, inflammatory cells (macrophages) predominate to a greater extent, it is more metabolically active and sensitive to lipolysis and insensitive to the effects of insulin compared to subcutaneous adipose tissue [14]. All this creates the preconditions for the adverse effect of visceral adipose tissue on both lipid and carbohydrate metabolism, and for local influence upon penetration into internal organs.
Since the outflow of blood from visceral adipose tissue occurs through the portal vein, hypertrophied adipocytes from visceral adipose tissue are associated with the appearance of high concentrations of free fatty acids and glycerol in the liver, resulting in a violation of their metabolism in this organ, in particular, a decrease in hepatic insulin extraction and increased production of triglycerides and glucose in the liver, which explains the association between visceral obesity and diabetes mellitus [15].
Thus, we are clearly beginning to understand that BMI is not of decisive importance in determining the severity of obesity, and risk stratification based on this indicator alone, especially in individuals with chronic CVD, is insufficient to assess the likelihood of developing obesity-related conditions, diseases, and their complications and outcomes. It becomes obvious that a certain pattern of distribution of adipose tissue, the predominance of visceral fat, morphological changes in visceral adipose tissue as part of the processes of remodeling and inflammation with the subsequent development of its dysfunction become the maximum role in increasing cardiometabolic risk in obesity. Based on the above, a more optimal classification of obesity should be developed in terms of its impact on the development and progression of CVD and assessment of individual cardiovascular risk [16].
conclusions
- The existing classification of obesity by degree does not take into account the accumulation of visceral adipose tissue, which has the most adverse effect on metabolic disorders and the risk of developing CVD.
- The degree of obesity does not reflect the severity of metabolic disorders, which play an important role as risk factors for the development of CVD.
- The accumulation of visceral adipose tissue is clearly associated with increased triglyceride and glucose levels and decreased HDL-C levels.
- The content of visceral adipose tissue of 16% or more is combined with an increase in triglyceride and glucose levels above normal values.
Literature/References
- Neeland IJ, Ross R, Després JP et al. Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: a position statement. Lancet Diabetes Endocrinol. 2019; 7:715–725. DOI: 10.1016/S2213-8587(19)30084-1.
- Dedov I.I., Melnichenko G.A., Shestakova M.V., Troshina E.A., Mazurina N.V., Shestakova E.A. and others. National clinical guidelines for the treatment of morbid obesity in adults. 3rd revision (Treatment of morbid obesity in adults). Obesity and Metabolism 2018; 15(1): 53–70. DOI: 10.14341/omet2018153-70. [Dedov II, Melnichenko GA, Shestakova MV, Troshina EA, Mazurina NV, Shestakova EA et al. Natsional'nyye klinicheskiye rekomendatsii po lecheniyu morbidnogo ozhireniya u vzroslykh. 3-iy peresmotr (Lecheniye morbidnogo ozhireniya u vzroslykh). [Russian National clinical recommendations for morbid obesity treatment in adults. 3rd revision (Morbid obesity treatment in adults).] Obesity and metabolism 2018; 15(1): pp 53-70. (In Russ.). DOI: 10.14341/omet2018153-70.
- National clinical guidelines for the diagnosis, treatment, prevention of obesity and associated diseases. St. Petersburg 2022 https://scardio.ru/content/Guidelines/project/Ozhirenie_klin_rek_proekt.pdf [Natsional'nyye klinicheskiye rekomendatsii po diagnostike, lecheniyu, profilaktike ozhireniya i assotsiirovannykh s nim zabolevaniy. Sankt-Peterburg 2017g.https://scardio.ru/content/Guidelines/project/Ozhirenie_klin_rek_proekt.pdf]
- Gonzalez-Muniesa P, Martinez-Gonzalez MA, Hu FB, et al. Obesity. Nat Rev Dis Primers 2017; 3: 17034. DOI: 10.1038/nrdp.2017.34.
- Després JP What is “metabolically healthy obesity”?: from epidemiology to pathophysiological insights. J Clin Endocrinol Metab 2012; 97:2283–85. DOI: 10.1210/jc.2012–2081.
- Neeland IJ, Poirier P, Després JP Cardiovascular and Metabolic Heterogeneity of Obesity: Clinical Challenges and Implications for Management. Circulation 2018; 137:1391–1406. DOI: 10.1161/CIRCULATIONAHA.117.029617
- Koster A., Murphy RA, Eiriksdottir G. et al. Fat Distribution and Mortality: The AGES-Reykjavik Study. Obesity 2015; 23, 893–897. DOI:10.1002/oby.21028.
- Scaglione R., Di Chiara T., Cariello T. et al. Visceral obesity and metabolic syndrome: two faces of the same medal? Intern Emerg Med (2010) 5: 111. DOI: 10.1007/s11739-009-0332-6.
- Druzhilov M.A., Druzhilova O.Yu., Beteleva Yu.E., Kuznetsova T.Yu. Obesity as a cardiovascular risk factor: emphasis on the quality and functional activity of adipose tissue // Russian Journal of Cardiology 2015, 4 (120): 111–117. DOI: 10.15829/1560-4071-2015-4-111-117. //Rossiyskiy kardiologicheskiy zhurnal 2015, 4 (120): 111–117. DOI: 10.15829/1560-4071-2015-4-111-117.]
- Cornier MA, Després JP, Davis N, Daurice A Grossniklaus DA, Klein S, Lamarche B et al. Assessing Adiposity A Scientific Statement From the American Heart Association. Circulation 2011;124: 1996-2019. DOI: 10.1161/CIR.0b013e318233bc6a.
- https://www.accessdata.fda.gov/cdrh_docs/pdf5/K052522.pdf
- Garvey WT, Mechanick JI, Brett EM, Garber AJ, Hurley DL, Jastreboff AM Reviewers of the kAACE/ACE Obesity Clinical Practice Guidelines. American Association of clinical Endocrinologists and American College of Endocrinology Comprehensive clinical practice Guidelines for medical care of patients with obesity. Endocr Pract, 22 Suppl 3, 1–203. DOI: 10.4158/EP161365.GL
- Grundy SM, Cleeman JI, Daniels SR et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005; 112:2735–52. DOI:10.1161/CIRCULATIONAHA.105.169404.
- Ibrahim MM Subcutaneous and Visceral Adipose Tissue: Structural and Functional Differences. ObesRev 2010; 11 (1): 11-18. DOI: 10.1111/j.1467-789X.2009.00623.x.
- Neeland IJ, Ross R, Després JP et al. Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: a position statement. Lancet Diabetes Endocrinol. 2019; 7:715-725. DOI: 10.1016/S2213-8587(19)30084-1.
- Chumakova G.A., Kuznetsova T.Yu., Druzhilov M.A., Veselovskaya N.G. Visceral obesity as a global cardiovascular risk factor // Russian Journal of Cardiology 2018; 23 (5): 7–14. DOI: 10.15829/1560-4071-2018-5-7-14. //Rossiyskiy kardiologicheskiy zhurnal 2018; 23 (5): 7–14. DOI: 10.15829/1560-4071-2018-5-7-14.]
S. V. Miklishanskaya*, 1, Candidate of Medical Sciences E. A. Zolozova*, Candidate of Medical Sciences A. A. Safiullina**, Candidate of Medical Sciences N. A. Mazur*, Doctor of Medical Sciences, Professor
* Federal State Budgetary Educational Institution of Further Professional Education RMANPE of the Ministry of Health of Russia, Moscow, Russia ** Federal State Budgetary Institution National Medical Research Center of Cardiology of the Ministry of Health of Russia, Moscow, Russia
1 Contact information
DOI: 10.26295/OS.2020.19.39.011
Visceral obesity in patients with different body mass indices / S. V. Miklishanskaya, E. A. Zolozova, A. A. Safiullina, N. A. Mazur For citation: Attending physician No. 8/2020; Issue page numbers: 66-70 Tags: obesity, cardiovascular disease, metabolic disorders
Causes of obesity in women
A woman becomes obese when her body stores more calories than it burns during the day and night. The human body needs calories (and essential vitamins, minerals, and other nutrients) to function properly and be active every day. But if a woman's body stores more calories than it burns, then the woman gains weight.
Researchers have noticed that a woman's environment throughout her life can influence the occurrence of obesity. While it's true that the food a woman eats is an important part of gaining or losing weight, other parts of her daily routine that she doesn't control can increase the likelihood of obesity.
Overweight and obesity affect women of all ages, races and ethnicities. But overweight and obesity are more common among certain groups:
- women from large cities;
- housewives;
- oriental women.
Many factors play a role in overweight and obesity, including marital status, past events and where a woman lives.
There are also some risk factors for overweight and obesity that a woman herself cannot control. But your doctor or dietitian may recommend changes to your eating habits and physical activity to help you achieve a healthier weight. Some medications may cause weight gain or make it more difficult to lose after treatment. If you suspect your medication is affecting your weight, you should talk to your doctor. You may need to try a different medicine.
Some medications can cause weight gain or make it difficult to lose. Photo: Pixabay
What to do
To achieve harmonious proportions, you need to balance your diet, that is, monitor the amount of carbohydrates, proteins and fats consumed. Most often, the problem is that we overindulge in sugar and other fast carbohydrates and do not consume enough food rich in protein and fiber.
Photo: istockphoto.com
To understand your diet, keep a special diary and write down everything you eat there. After a week, you will be able to see the full picture of your diet - how many calories, proteins, fats and carbohydrates you consume - and find where the imbalance lies in your diet. Based on this, it will be possible to create a healthy, balanced menu. The main rule is to eat less sweets, more vegetables, grains and lean protein foods and lead a more active lifestyle.
How to get rid of the feeling of hunger? 10 healthy snack ideas
However, proper nutrition and exercise cannot always help with excess weight. Perhaps your obesity is not just the result of overeating, but a sign of serious health problems. In this case, you should check your hormonal levels and consult a doctor.