Sternocleidomastoid muscle[edit | edit code]
Sternocleidomastoid muscle
Sternocleidomastoid muscle
(
m. sternocleidomastoideus
) tilts the head and cervical spine in the same direction and, with unilateral contraction, rotates them in the opposite direction. With bilateral contraction there is no rotation. Flexion and extension of the neck depends on the initial position of the head. If the head is flexed, this muscle further flexes the head and cervical spine; if the head is extended, the muscle further extends the head and cervical spine. The effect of this muscle on the sternum and collarbone is insignificant.
Home[edit | edit code]
- Sternal head: manubrium of the sternum
- Clavicular head: medial part of the clavicle
Attachment[edit | edit code]
- Mastoid
Innervation[edit | edit code]
- Accessory nerve (XI pair of cranial nerves), cervical plexus, C2
Functions[edit | edit code]
| Synergists | Antagonists |
| Atlanto-occipital joint | |
| Flexion (with the head bent) | |
| m. rectus capitis anterior, m. longus capitis, m. scalenus anterior, mm. suprahyoidei, mm. infrahyoidei | Deep muscles of the back of the neck, which attach to the head m. sternocleidomastoideus (with the head extended) m. levator scapulae m. trapezius (descending part) |
| Extension (with the head extended) | |
| m. semispinalis capitis m. longissimus capitis m. splenius capitis m. levator scapulae m. trapezius (descending part) | m. rectus capitis anterior m. longus capitis mm. suprahyoidei mm. infrahyoidei |
| Atlantoaxial joint | |
| Rotation in the opposite direction | |
| m. trapezius (descending part) All muscles acting as antagonists on the same side become synergists when contracted on the opposite side | m. longissimus capitis m. splenius capitis m. rectus capitis posterior major m. obliquus capitis inferior All muscles acting as antagonists on the same side become synergists when contracted on the opposite side |
| Intervertebral discs and joints (cervical) | |
| Flexion (with the head bent) | |
| m. longus colli, m. longus capitis, m. scalenus anterior, mm. suprahyoidei, mm. infrahyoidei | Deep muscles of the back of the neck m. levator scapulae m. trapezius (descending part) |
| Extension (with the head extended) | |
| m. semispinalis capitis, m. longissimus capitis, m. splenius capitis, m. levator scapulae, m. trapezius (descending part) | m. rectus capitis anterior, m. longus capitis, m. longus colli, m. trapezius (descending part), m. scalenus anterior |
| Intervertebral discs and joints (cervical), atlanto-occipital and atlanto-axial joints | |
| Tilt in the same direction | |
| m. splenius capitis, m. longissimus capitis, m. rectus capitis lateralis (atlanto-occipital joint only), mm. scaleni, m. trapezius (descending part), m. levator scapulae | All muscles acting as antagonists on the same side become synergists when contracted on the opposite side |
Neck extension. Functional muscle tests[edit | edit code]
Clinical relevance
- With unilateral contraction of the sternocleidomastoid muscle, torticollis develops.
- Contraction of the sternocleidomastoid muscle can increase cervical lordosis by moving the head forward relative to the cervical spine and flexing the cervical spine relative to the thoracic spine.
- The sternocleidomastoid muscle is one of the accessory respiratory muscles. It is better to test on a smooth surface.
Issues and comments
- The short muscles of the neck area (neck extensors) are also involved in this movement.
- To test the sternocleidomastoid muscle on one side, it is necessary to rotate the head in the direction opposite to the side being tested.
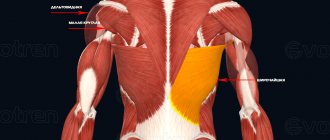
Muscle anatomy
The paired structure is located symmetrically on the anterolateral surfaces of the neck deeper than the subcutaneous muscle. It has an oblique spiral-like stroke, which you can trace yourself by turning your head in any direction. In this case, the muscle will be clearly contoured in the form of a dense and relatively narrow cord, which can be grasped with your hands along almost the entire length.
The anatomy of the sternocleidomastoid muscle connects several skeletal structures:
- sternum;
- both collarbones;
- skull bones: temporal and occipital.
Consists of two heads: lateral and medial. The first starts from the collarbone, its sternal end. The second is from the anterior surface of the manubrium of the sternum. They go obliquely upward and backward, connecting behind the ear. Here they are attached to the mastoid process of the temporal bone and to the superior nuchal line on the occipital bone. Moreover, the fibers of the medial part lie higher than those of the lateral part.
At the point of origin, the legs form several pits. Two of them are symmetrical and represent a depression between both portions of the muscle, called the small supraclavicular fossa. Finger pressure here helps stop bleeding from the subclavian artery, as well as diagnose phrenicus, a symptom that signals inflammation of the gallbladder. The third, jugular fossa, is located between the adjacent medial legs.
Nutrition, innervation and lymphatic drainage
The sternocleidomastoid muscle, located on the anterior surface of the neck, receives blood supply from several arterial basins. Main branches:
- the sternocleidomastoid branches of the occipital artery from the external carotid feed predominantly the upper half;
- The superior thyroid artery, also arising from the external carotid, is the source of nutrition for the lower half.
Venous outflow is carried out by veins of the same name: the occipital flows into the external jugular, less often into the internal; The superior thyroid vein flows into the facial or internal jugular vein.
Innervation is carried out through the accessory nerve, an alternative name is the XI pair of cranial nerves, as well as the motor branches of the cervical plexus (in Latin, plexus cervicalis).
Lymph from the sternocleidomastoid muscle is collected in several groups of lymph nodes: the mastoid, which collects it from the upper part, and the superficial cervical. All of them flow into deep nodes of the neck, forming symmetrical jugular trunks.
Torticollis in children surgery and treatment.
Torticollis
Types and causes, Treatment of torticollis
Torticollis is a group of diseases that are similar in clinical manifestations, but have different causes. A change in the shape of the neck can occur with damage to any of its anatomical structures, but most often occurs with pathology of the sternocleidomastoid muscle. This muscle is paired, one end is attached to the mastoid process of the skull behind the ear, and the other to the collarbone. Its function is tilting the head with a turn, circular movements of the head.
Types and reasons
Torticollis can be congenital or acquired. Congenital torticollis appears in the prenatal period as a result of an infectious disease of the mother or fetus, pathology of the structure of the mother’s pelvis, abnormal position of the fetus relative to the pelvis, genetic and chromosomal diseases. Acquired torticollis can appear as a result of pathological childbirth due to injury to the neck muscles, dislocation, ischemia, entanglement of the umbilical cord, and can occur at a later age due to infection, trauma, or diseases of the nervous system.
Types of congenital torticollis
Idiopathic
torticollis is manifested by a slight unfixed tilt of the head towards the affected sternocleidomastoid muscle and a turn in the opposite direction. The reasons for the development of the pathology are not clear, but it has been noted that it often develops in infants whose mothers had a pathological pregnancy and complicated childbirth. When palpated, the affected muscle is tense, its shape and length are unchanged. Often idiopathic torticollis is combined with perinatal encephalopathy and segmental insufficiency of the cervical spine.
Myogenic congenital
– occurs as a result of organic damage to the sternocleidomastoid muscle, clinically expressed by its shortening and thickening. More often, a rounded compaction is palpated at the border of the lower and middle third of the muscle, or the muscle is compacted evenly and takes on the appearance of a spindle. There are early and late forms of myogenic torticollis. The early form appears immediately after birth, the late form - in the third or fourth week of life. With prolonged forced positioning of the head in utero, or pathology in the development of muscle fibers and tendons, muscle function is disrupted and torticollis develops. Such conditions can occur with a breech presentation of the fetus, or a transverse position in the uterus with the head adducted to the shoulder. In this case, muscle fibrosis occurs and it becomes inelastic. The head is tilted towards the shoulder on the side of the affected muscle and turned in the opposite direction. Any attempts to change the position of the head bring pain to the child. A forced position leads to disruption of the development of bones and muscles of the skull, shoulder girdle, and to curvature of the spine. The face becomes asymmetrical: on the affected side, the eyes, eyebrows and ears are lowered, the bones are flattened. In addition to unilateral muscular torticollis, bilateral muscle torticollis sometimes occurs when both sternocleidomastoid muscles are affected. In this case, the patient's head is brought to the sternum and movements of the neck and head are sharply limited.
Osteogenic congenital
– occurs as a result of pathology of the cervical vertebrae. Klippel-Feil disease is manifested by the fusion of the cervical vertebrae into a monolithic block, which impairs mobility in the cervical spine, or the vertebrae are not fused, but their number is less than normal, or their size is smaller. The neck is significantly shorter than normal, deformed with a bend in one direction. This disease can be combined with other congenital skeletal defects, which aggravates the overall clinical picture. More often, the pathological structure of the neck does not cause pain to the child, but radiculitis of the cervical spine (pinched nerves) is possible, which is difficult to correct. Appearance of a child with osteogenic congenital torticollis: low-set head (pulled into the shoulders) often turned to the side, low hair growth on the back of the head, limited mobility in the cervical region.
Neurogenic congenital
torticollis becomes a consequence of the development of dystonic syndrome. The syndrome is manifested by increased skeletal muscle tone on one side and decreased tone on the other (left or right). In this case, the tension manifests itself equally in the upper and lower limbs. On the affected side, the handle is clenched into a fist, the leg is bent. When the child is positioned on his stomach, the head is turned to the affected side, the spine takes the shape of an arc. Movements in the cervical spine are fully preserved.
Arthrogenic
– as a result of rotational subluxation of the atlantoaxial joint. The child's head is tilted to one shoulder and turned to the other, movements in the cervical spine are sharply limited and painful. It can be either congenital or acquired.
Types of acquired torticollis
Attitudinal - occurs as a result of consolidating the stereotype of the child’s position lying in bed or in the arms of an adult. There are no organic lesions of the spine or muscles.
Torticollis due to paralytic strabismus. The position of the head is formed due to gaze fixation, while the extraocular muscles are completely or partially deprived of their function. The range of motion in the cervical spine is not limited, palpation is painless.
Dermatogenic – develops as a result of scarring changes on the skin after injuries and burns. The scars tighten the skin and cause a fixed position of the head.
Desmogenic - develops as a result of inflammatory processes in the tissue and lymph nodes of the neck. Atrophic and scarring changes change the position of the head and neck.
Myogenic – as a result of inflammation of the neck muscles followed by their organic change.
Neurogenic acquired - develops as a result of a previous neuroinfection or cerebral palsy.
Traumatic osteoarticular – caused by a fracture of the body of the first cervical vertebra, the atlas. Movement in the cervical spine is limited and very painful. Palpation of the back of the head and neck causes severe pain. The baby is restless and does not latch well. Neurological examination reveals bulbar syndrome, pyramidal insufficiency. More often it is acquired.
Grisel's disease is a subluxation of the atlas (first cervical vertebra) caused by inflammation of the soft tissues of the pharynx or pharynx. Occurs in children aged six to ten years. It appears unexpectedly, expressed by tilting the head to the shoulder.
Infectious diseases of the bones of the spine can lead to melting or fracture of the cervical vertebrae. The cause may be osteomyelitis, syphilis, tuberculosis.
Torticollis as a result of a malignant or benign tumor of the spine.
Hysterical torticollis is an unnatural turn of the head that develops against the background of hysterical psychosis.
Treatment of torticollis
The treatment program for congenital myogenic torticollis at an early stage includes massage, corrective exercises, and physiotherapeutic procedures. The technique of massage and correction will be discussed below. Physiotherapy includes thermal procedures, electrophoresis. Dry heat is prescribed from the moment the pathology is detected. Electrophoresis with potassium iodide and lidase - in the seventh to ninth week of life.
In case of late diagnosis, or lack of effect from conservative treatment, an open intersection of the heads of the sternocleidomastoid muscle is performed. This operation is quite simple, the prognosis for recovery is favorable.
If the difference in the length of the affected muscle and the opposite healthy one is more than forty percent, plastic surgery is performed to lengthen it.
The optimal age for the operation is five years. After the operation, a plaster cast is applied from the chest to the chin in front and from the shoulder blades to the back of the head. A month later, the bandage is changed to Shants’ collar and physiotherapy, massage, and exercise therapy are prescribed.
Treatment of acquired myogenic torticollis is similar to the treatment of congenital torticollis. In adult patients, the surgical method is more often used, due to the less plasticity of the musculoskeletal system.
Congenital neurogenic torticollis is treated with drugs that reduce muscle tone and excitability of the nervous system. General and local massage, exercise therapy, and physiotherapy are also prescribed.
If the cause of torticollis is a dislocation or injury to the bone, this pathology is eliminated using orthopedic and surgical methods. These measures are usually sufficient. If the injury has existed for a long time and organic changes have occurred in the muscles of the neck, shoulders, and spine, additional conservative treatment is prescribed: massage, exercise therapy, electrophoresis, electric pulse therapy, etc.
Torticollis due to neuroinfection is corrected after elimination of active inflammation. Antibiotics, anticonvulsants and muscle relaxants are prescribed. In the future, wearing a Shants collar and exercise therapy is indicated. In severe cases of spasm, surgery is prescribed.
Treatment of Klippel-Feil disease is aimed at normalizing cerebral circulation and stimulating the development of the muscles of the neck and upper limbs. For radiculitis, the pinched nerves are transected.
Treatment of Grisel's disease. At the inflammation stage, antibiotics and anti-inflammatory drugs are used. Subsequently, neck traction using a Glisson loop.
Dermatogenic and desmogenic torticollis are subject to surgical treatment. Damaged tissue is excised and replaced with allo- or xenografts.
Bone infections are eliminated through specific and nonspecific antibiotic therapy, followed by surgical bone restoration.
Massage and corrective exercises for myogenic torticollis in children under one year of age.
Since the most common cause of torticollis is damage to the sternocleidomastoid muscle, and it is this pathology that can be treated with massage and gymnastics, special attention should be paid to this topic.
It is better to massage babies with the hands of the mother, and her preliminary training is necessary. Since with torticollis, not only the damaged muscle suffers, but also the healthy one on the opposite side, both sternocleidomastoid muscles should be massaged. The massage begins on the healthy side in order to increase the tone of the overstretched and weakened muscle. The index, middle and ring fingers make circular movements without effort, along the muscle from the ear to the collarbone. After this, they move to the affected side. Apply light stroking movements along the muscle in the direction from the ear to the collarbone. The second stage is smoothing: from the compaction in both directions along the muscle, movements are made with the index finger up, and the middle and ring finger down. The position of the head should ensure the most relaxed state of the sternocleidomastoid muscle. The duration and intensity of the massage should be adjusted according to the condition of the affected muscle: as tension increases, the massage should be short and gentle. The purpose of the massage is to increase blood flow in the affected muscle and stimulate recovery processes.
After the massage, corrective exercises should be performed. The correction is aimed at restoring the proper length of the affected muscle and giving it elasticity. All movements should be smooth and easy to prevent the pathology from worsening. The position of the child is lying on his back. First, the shoulder on the affected side is fixed in the correct position, after which they begin, gradually shaking, to tilt the head towards the healthy shoulder. When the tilt has reached the maximum possible at this stage, the head is also gradually and smoothly turned in the direction of the lesion. You should hold your head and shoulder in the maximum correction position for 15 seconds. Exercises are carried out for 10-15 minutes five times a day.
Positional correction is carried out throughout the day. The child is positioned relative to the light source so that there is an optimal tilt and rotation of the head. Laying on the stomach with the head turned towards the affected side. Position on the arms of an adult with optimal tilt and turn of the head.
To maximize the effect and prevent complications, you should strictly adhere to the technique and sequence of correction steps. To consolidate the achieved effect, it is recommended to wear a Shants collar.
Consequences of untreated torticollis
The negative consequences of both congenital and acquired torticollis increase in direct proportion to the time of existence of the pathology. In childhood, persistent pathological tilt of the head leads to dystrophic changes in the neck muscles and degeneration of muscle tissue into connective tissue. The development of the facial skull is disrupted: the bones on the affected side are smaller and flattened, the palpebral fissure is smaller, the auricle and eyebrow are lowered, and with age the face becomes more and more asymmetrical.
The neck contains large vessels that carry blood circulation to the brain. Prolonged compression of them by a forced position of the neck initially leads to disruption of the cerebral outflow of blood, which leads to the development of migraine-type headaches. Subsequently, the obstructed flow of arterial blood to the brain affects the brain: brain functions in adults (memory, attention) are impaired, and intellectual development in children suffers.
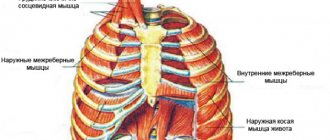
The function of external respiration is impaired, as the position of the trachea changes, and one part of the chest lags behind in development.
Due to chest deformation, cardiac activity is impaired.
Chronic inflammation of the paranasal sinuses and ear on the affected side develops as a result of impaired mucus outflow.
Speech is impaired, strabismus develops, vision decreases, and hearing suffers.
from the site medical reference book - Doctor's Book
Treatment of torticollis
Treatment for torticollis includes: therapeutic massage, therapeutic, corrective gymnastics, positional treatment, and physiotherapy. Of particular importance for torticollis is passive corrective gymnastics, which helps lengthen the fibers of the affected sternocleidomastoid muscle.
Using careful techniques, without violence, the nurse tilts the child’s head in the healthy direction and at the same time turns his face in the opposite direction.
The child’s shoulders should be pulled down as far as possible and fixed to the bed to prevent the attachment points of the sternocleidomastoid muscle from approaching. To obtain the greatest effect, corrective exercises should be carried out by two people: one does the gymnastics, the other fixes the shoulders and chest. Any violent movements must be excluded in this case.
Otherwise, tears or even ruptures of muscle fibers may occur, which, ending in scarring, worsen torticollis. In addition, such manipulations can cause severe neurotic conditions in children. Treatment by position: the child should lie on a semi-rigid mattress without a pillow. Sometimes a diaper folded several times is placed under the head. Light, toys, communication with adults should be on the side of the torticollis. You can position your baby using a rubber ring wrapped in cloth and placed under the back of the head. You can also place the child in a corrective position using two bags (size 20 by 30 cm) with sand (salt, cereal), which are placed on both sides of the head or on the side of the torticollis (above the shoulder girdle). This is a very effective positioning, mainly in the first months of a child’s life, when it is impossible to cause active corrective movements of the child’s head. The sand evenly fills the voids in the neck area, thereby gently correcting the correct position of the head. A prerequisite is the correct position of the entire body.
It should be symmetrical, straight to the head. To do this, you can put bags or roll up a roll of blanket and place it from the armpits to the child’s knees. This styling should be done for 2-3 daytime naps. It is better to leave the child alone at night. The nurse should be close to the child and monitor his condition. Frequent regurgitation excludes the proposed placement. The child should be placed on his side more often. On the side of the torticollis, a high pillow is placed under the head. If the child is lying on the healthy side, then the pillow is not used at all. A number of authors (for example, M.V. Alder) recommend using cotton-gauze pads, which are bandaged on both sides of the neck and tied through the armpits of the opposite sides. From three to four weeks of age, to make the pillow more durable, a strip of cardboard is inserted into the pillow, the width of which is equal to the distance between the lower jaw and the collarbone with the head in the correct position. As for cotton-gauze pads, bandages with traction and various collars recommended for holding the child’s head in the correct position, they easily bring the attachment points of the shortened muscle closer together due to raising the shoulder on the side of the affected sternocleidomastoid muscle and tilting the head back. These movements, which the child strives for due to unpleasant sensations in the stretched muscle, are not inhibited by anything, which is a significant drawback of these techniques. It is important to carry the baby correctly in your arms.
Taking the child in an upright position, press him with his chest towards you (facing him).
The adult's shoulders and the child's shoulders should be at the same level. Turn the baby's head to the painful side and fix this position with your cheek.
Take the child with his back to you; With your cheek, turn his head to the painful side and tilt it slightly. Carry the child on his side with the sore side down and hold his head with your hand, lifting him to the healthy side.
of torticollis should be
It is properly organized, taking into account all the characteristics of the child’s body.
Improper organization of it adversely affects the general condition of the child and delays the correction of torticollis.
It is important to follow a certain sequence in the procedures. Thus, it is more advisable to carry out massage and electrophoresis on different days. You should not massage immediately after electrophoresis, as this promotes the excretion of potassium iodide ions.
Unlike massage and electrophoresis, thermal procedures and especially passive corrective gymnastics must be performed daily; in this case, there is a constant lengthening of the fibers of the shortened muscle, an increase in the tone of the same muscle on the opposite side of the neck and consolidation of the correction achieved through treatment. In particularly severe forms of congenital muscular torticollis, when the compaction covers half or more than half of the sternocleidomastoid muscle, even early and correctly carried out treatment does not always lead to elimination of the deformity. In such cases, complete cure can only be achieved through surgery.
Surgical treatment is indicated after the age of one year,
but due to the difficulty of postoperative treatment, practically the operation should be performed after the age of three.
During surgical treatment, the pedicles of the sternocleidomastoid muscle are dissected and excised for at least 2 cm, and the fascia of the neck wrinkled on the side of the lesion is also dissected.
After the operation, the head is fixed with a Glisson loop so that it is tilted towards the healthy side and turned towards the postoperative wound. The Glisson loop is a special device in the form of a fabric collar covering the neck, chin and back of the head. A load is suspended from the top of the loop, the thrust of which is thrown through the block.
During the period of traction with the Glisson loop, head movements, movements in the shoulder joints, and sudden movements of the legs are contraindicated. In some cases, after surgery, the head and torso are fixed with a circular plaster cast, consisting of a plaster corset and a head holder. The headband holds the head in the correct position, and sometimes even in an overcorrected position.
In bed, a patient with a plaster cast needs to create an elevated position, for which 2-3 pillows are placed under the head. After removing the plaster cast and/or Glisson loop, the head is fixed with a Shants collar made of plastic, and corrective gymnastics is prescribed.
The results of timely treatment of torticollis are favorable.
Despite a satisfactory immediate result, treatment should not end before a year. It should be taken into account that the affected sternocleidomastial muscle is stunted in growth compared to the same muscle on the opposite side. Treatment can be considered complete only if there is a slight overcorrection of the deformity, i.e., when by the time the treatment is completed, the affected muscle is slightly longer than the healthy one.
A slight hypercorrection observed at one or two years of age should not cause concern, since by the end of the growth of the sternocleidomastial muscles, their length evens out. Treatment should be comprehensive, systematic, with the obligatory involvement of parents, since it is they who need to be told and shown fixing techniques and positions that help restore muscle function.
Upon discharge from the hospital, it is necessary to consult parents about the child’s orthopedic regimen:
At home and at school, you need to ensure that children after surgical treatment for muscular torticollis sit down at their desks during games or activities so that their heads turn towards the torticollis.
In this case, the child, distracted, turns his head to the side and stretches the shortened neck muscle.
It is necessary to teach your child to sleep on his side; sleep on the side of the torticollis with the obligatory placement of a bolster or a high pillow under the head, do not use a pillow on the healthy side, i.e. if the torticollis is on the right, then sleep on the right side will be with a pillow, on the left - exclude the pillow.
Technique of surgery for torticollis
The child is placed on the operating table with a cushion placed under the shoulder blades and the head is turned to one side. The operation is performed under general anesthesia. Supraclavicular sections of the skin, m.platysma myoides and fascia expose the clavicular and sternal legs of the distal tendon of the sternocleidomastoid muscle. One by one, a Kocher probe is placed under them and opened.
It is necessary to operate very carefully so as not to injure the internal jugular vein, especially when it is necessary to open the fascial sheath of the muscle in order to more easily correct the position of the head. In all cases, both legs of the tendon should be divided, not just one.
In girls, in order not to form a scar above the collarbone, the proximal tendon at the mastoid process is crossed. Here, too, caution is necessary, since the external jugular vein, n.accesorius and n.facialis are nearby. Therefore, the muscle should be slowly separated and the tendon should be exposed 1 cm below the apex of the mastoid process. During surgery for torticollis, the position of the head is corrected, hemostasis is performed and the wound is sutured. After tenotomy, the position of the head is corrected and fixed with a plaster thoraco-cranial bandage.
This bandage is applied with the child in a sitting position, and it can be difficult to properly record the degree of correction achieved when the child recovers from anesthesia. Therefore, after the operation, a Glisson loop is applied for 2-3 days, and then a plaster cast is applied. If repeated correction is required, then cut the bandage around the neck (if necessary, using wedges), increase the tilt of the head and plaster the section area with a bandage. If necessary, the correction can be repeated after three to four days.
The same manipulations are carried out in the Matzen bandage, however, this bandage is less stable and is not very beneficial when the child is lying down. During your stay in a plaster cast at the site where the tendons are opened, the hematoma becomes scarred and the scar thickens. The plaster cast is removed after 4-5 weeks and rehabilitation treatment begins.
Neck muscle massage, corrective exercise therapy for torticollis, thermal procedures and a corrective collar are prescribed. Sometimes corrective traction of the spine with a Glisson loop is used. It is important to teach your child to hold his head correctly.
Postoperative conservative treatment is carried out for 2-2.5 months.
Recurrences of torticollis occur only in those patients in whom both legs of the tendon and cicatricial adhesions were not crossed or proper hemostasis was not performed.
Speaking about surgery for torticollis, we should mention the plastic continuation of the sternocleidomastoid muscle, once developed by Iosiegi. The operation consisted of separating both legs of the muscle, and then cutting off the clavicular leg at the collarbone and cutting off the sternal leg at the muscle.
After installing the head in hypercorrection, the ends of the distal tendon legs were sutured together.
Today no one performs this operation for torticollis, as well as the operation proposed by Mikulic - resection of part of the pathologically altered muscle.
As already mentioned, if the child is not treated or does not adhere to the recommendations of the orthopedist, then bone torticollis, facial asymmetry and “scoliosis” of the skull occur, which are irreversible and remain for life. come back
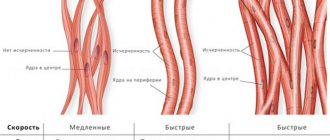
Trigger points
Trigger points are points or areas on a muscle that are highly irritable. Their excitation may be associated with persistent myofascial pain syndrome and certain complaints from other organs.
Trigger points of the sternocleidomastoid muscle:
- Those located in the lower part cause pain localized in the upper parts of the sternum, and also contribute to the appearance of paroxysmal dry cough.
- Points in the middle part of the medial fasciculus cause pain in the upper jaw, orbit and supraorbital region.
- Located on the inner edge of the medial crura, they irritate the pharynx, causing soreness and soreness, as well as discomfort in the back of the tongue.
- Points in the area where the muscle attaches to the skull cause pain in the back of the head.
- Triggers in the middle of the lateral fasciculus project pain sensations to the frontal region;
- Irritation of the points of the upper part of the lateral crus contributes to the appearance of discomfort in the depths of the ear.
To date, the medical community has not definitively proven the objectivity of identifying trigger points and the dependence of symptoms due to the small number of reliable studies. However, this knowledge is widely used in massage and acupuncture, causing positive effects in patients.