Anatomy
At the high school level, they begin to take a human anatomy course. This is a very interesting and at the same time extensive section of biology, requiring the acquisition of high-quality knowledge. Human anatomy is a science that examines the structure of the body, its functions and life activities in general.
A skeletal model or anatomical atlas will tell you where the human forearm is located. By carefully studying the name, location, types and purpose of bones, it is easy to understand the structure of the human upper limb - the hand.
Skeletal mobility is provided by muscles attached to bones. Looking at the forearm, where there are many different types of muscle tissue, can give you an idea of how the arm moves. Muscle contraction is facilitated by nerve impulses received by nerves located in the forearm.
Forearm: where is it located? Photo of a human skeleton
So, a little theory. An anatomical atlas or a skeleton model will help answer the question of where the human forearm is located. The bones of the forearm are one of the components of the human upper limb, which plays an important role in the mobility of the arms. By carefully studying the skeleton image, it is easy to see where the shoulder and forearm are located.
From the name you can guess that the forearm is located under the humerus bones, precedes it and together forms the basis of the upper limb of a person. To understand the anatomy of the upper limb, it is necessary to study the bones that make it up.
Damage Prevention
Prevention measures include, first of all, minimizing injuries. To do this you need:
- In icy conditions, wear shoes with non-slip soles.
- Athletes must wear protective equipment.
- Observe safety precautions in production.
Strengthening the ligaments and muscles of the upper limb is of great importance. To do this, you should regularly exercise, swim, and spend more time in the fresh air. Proper nutrition is also an essential part of prevention. The diet should have enough protein and minerals, especially calcium, magnesium, phosphorus and zinc.
With age, to maintain the shock-absorbing function of cartilage, it is recommended to take chondroprotectors. The bones of the forearm perform many important functions in human life. Any injury or illness requires timely consultation with a doctor and qualified treatment.
Bones of the forearm
Part of the upper limb - the forearm, where two bones are located, has a fairly simple structure. It consists of long tubular bones: the ulna and radius, each of which has its own structural features.
What you need to know about the structure of tubular long bones:
- They consist of the diaphysis, metaphysis and pineal gland. The diaphysis is a moderately elongated part of the bone, having a cylindrical or triangular shape. Metaphysis is the space between the diaphysis and the pineal gland. The pineal gland is the thickened end needed to connect to the joint.
- The articular surface is located on the epiphysis, which is covered with articular cartilage.
- The epiphyses, depending on the position of the bone, can be proximal (upper) and distal (lower).
- It is due to the metaphysis and the cartilaginous tissue located on it that tubular bones grow in length.
- The epiphysis is spongy, the diaphysis is compact.
The body of the ulna and radius are triangular in shape, meaning they have three surfaces. The front of the bone faces forward, and the back - back. The position of the third side is different on the radial and ulnar sides.
Operations
Access to the diaphysis of the radius can be made along the outer, palmar or dorsal side of the radius; access to the diaphysis of the ulna is along the inner, palmar plate of the back side of the P. The ulnar artery and ulnar nerve are exposed using the palmar-ulnar approach. When the skin is supinated, the skin incision is made from the medial epicondyle of the humerus to the outer edge of the pisiform bone. After dissecting the fascia, the ulnar artery and ulnar nerve are located in the space between the flexor carpi ulnaris and the flexor digitorum superficialis. The radial artery and superficial branch of the radial nerve are exposed using the palmar radial approach. A skin incision is made with the P. in a supinated position along the line connecting the outer edge of the biceps brachii tendon and the styloid process of the radius. The artery and superficial branch of the radial nerve are exposed between the pronator teres and the brachioradialis muscle.
For osteosynthesis (see) of P.'s bones, plates, pins, and distraction-compression devices are used (see).
Amputation of the forearm in the upper and middle third is carried out using a patchwork or circular method with a cuff. The median, ulnar and radial nerves are shortened by 4-5 cm in order to exclude the possibility of the formation of an amputation neuroma under the skin at the end of the stump. Muscles and tendons are crossed in the same plane 3-4 cm distal to the bone sawdust. P.'s bones are filed down at the same level, their edges are smoothed with a rasp. The vessels are ligated with catgut (see Amputation). According to indications, kinematization of the stump is carried out (see Krukenberg hand). Resection of P.'s bones is carried out for tumors, in some cases of osteomyelitis and false joints.
Lengthening of P.'s bones is indicated for clubhandedness (see), congenital and acquired shortenings. After an oblique osteotomy, lengthening is performed using distraction-compression devices. Osteotomy in the P. area is similar in indications and technique to osteotomy of other long tubular bones (see Osteotomy).
Bibliography:
Kaplan A.V. Damage to bones and joints, p. 252, M., 1979; Kaptelin A. F. Rehabilitation treatment (physical therapy, massage and occupational therapy) for injuries and deformations of the musculoskeletal system, M., 1969; Clinical X-ray anatomy, ed. G. Yu. Koval, p. 199, Kyiv, 1975; Kovanov V.V. and Travin A.A. Surgical anatomy of the upper extremities, M., 1965; Maykova-Stroganova V. S. and Rokhlin D. G. Bones and joints in x-ray images, Limbs, p. 331, L., 1957; Multi-volume guide to orthopedics and traumatology, ed. N. P. Novachenko, vol. 1, p. 389, M., 1967, vol. 2, p. 483, 515, M., 1968; Nagy D. X-ray anatomy, trans. from Hungarian, p. 74, Budapest, 1961; Operative surgery and topographic anatomy, ed. V.V. Kovanova, p. 29, M., 1978; Experience of Soviet medicine in the Great Patriotic War of 1941-1945, vol. 15, p. 276, M., 1952; Essays on military field surgery, ed. Yu. G. Shaposhnikova, M., 1977; Reinberg S. A. X-ray diagnosis of diseases of bones and joints, book. 1-2, M., 1964; Rubasheva A. E. Private X-ray diagnostics of diseases of bones and joints, Kyiv, 1967; Chernavsky V. A. Diagnosis and treatment of fractures and dislocations, p. 96, Tashkent, 1977; Bensahel N. Fractures de Monteggia, Rev. Prat., v. 22, p. 1679, 1972; Boileau F., Preaut J. et Malka G. Les fractures diaphysaires récentes de l'avant-bras chez l'adulte, Ann. Med. Nancy, t. 12, p. 2257, 1973, bibliogr.; Brug E., Beck H. u. Heuwieser R. Osteosynthese son Unterarmschaftfrakturen mit dem Bündelnagel nach Hackethal, Chirurg, Bd 46, S. 113, 1975; Christensen NO Küntscher intramedullary reaming and nail fixation for nonunion of the forearm, Clin. Orthop., v. 116, p. 215, 1976; Eaton RG a. Green WT Volkmann's ischemia, A volar compartement syndrome of the forearm, ibid., v. 113, p. 58, 1975; Erler F. Osteosynthesen bei Unterarmbrüchen, Beitr. Orthop. Trau-mat., Bd 23, S. 132, 1976; Finkbeiner GF u. Hort W. Therapie der anbehandelten Unterarmfrakturen, Z. Orthop., Bd 114, S. 666, 1976; Lanz T.u. Wachsmuth W. Praktische Anatomie, Bd 1, B., 1959; Lukäcs L. u. Törtely E. Komplikationen nach Verplattung von Unterarmbrüchen, Akt. Traumatol., Bd 6, S. 221, 1976.
CC Tkachenko; V. P. Illarionov (medical phys.), M. K. Klimova (rent.), E. R. Mattis (surgery), A. A. Travin (an.).
The structure of the ulna
We have already understood that in the forearm there are two long tubular bones connected on both sides by joints. The third side of the ulna is called the medial side and faces inward, like its edges.
The ulna is located on the outside of the arm, which is called the medial position. For example, if we consider a limb on the left and right, the left forearm contains the ulna on the left and the right on the right. In other words, the ulna is located in the forearm on the little finger side.
The superior epiphysis of the ulna is thicker than the proximal epiphysis of the radius and articulates with it through a block-shaped depression, which is limited by two processes: the coronary and ulnar. On the inner side of the coronoid process there is a radial notch intended for the radial capital. The joint, together with the articular surface and cartilage, forms the elbow joint, which allows flexion and extension of the forearm.
The lower epiphysis, on the contrary, is thinner than the distal epiphysis of the radius and is connected to it using an articular circumference, and then passes into the wrist joint.
Pathology
Developmental defects
are rare. These include: hemimelia - complete absence of the entire forearm; phocomelia - underdevelopment of the shoulder and hip, when the hand starts directly from the body; peromelia - the complete absence of the entire upper limb, when a slight rudiment extends from the body. Congenital absence or underdevelopment of the radius or ulna is often symmetrical and entails congenital clubhand (see).
Congenital dislocation of the radius develops due to pathological shortening of the ulna with a normal length of the radius. The head of the radial bone is usually deformed, which is associated with limited rotation, flexion and extension of the radius. Surgical treatment is resection of the head of the radial bone in patients over 14 years of age.
P.'s developmental defects also include congenital radioulnar synostosis (see Elbow joint) and Madelung's disease (see Madelung's disease).
Damage
P. can be closed or open. Closed injuries include bruises (see), ruptures of muscles and tendons (see Distortion, Muscles), as well as bone fractures (see Fractures). With significant subfascial hematomas due to P.'s bruises, compression of blood vessels, nerves and muscles is possible, which is manifested by ischemia, impaired skin sensitivity and hand function. In these cases, an incision of the skin and fascia and removal of the hematoma are indicated. Subcutaneous ruptures of the muscles and tendons of the P. are rare.
They can be complete or partial. Diagnostic signs are local pain, hematoma, dysfunction of the hand or fingers. For partial damage, conservative treatment is indicated. Complete ruptures are subject to surgical treatment with suturing of the damaged muscle or tendon.
In case of injuries to soft tissues of P., primary surgical treatment of wounds is performed (see).
Fractures of the forearm bones among all bone fractures range from 5 to 25%. They can be open or closed.
Fractures of the head of the radius, olecranon, coronoid process of the ulna - see Elbow joint.
Rice.
4. Radiographs of the forearm with Monteggia (a) and Galeazzi (b, c) fractures: a - comminuted fracture of the ulna in the proximal third with dislocation of the head of the radius; b — fracture of the radius in the middle third with dislocation of the head of the ulna; c — fracture of the radius, dislocation and fracture of the head of the ulna (variant of the Galeazzi fracture). Rice. 5. Direct (a) and lateral (b) radiographs of the forearm bones with a subperiosteal fracture in a child.
Fractures of the diaphysis of the forearm bones occur due to direct or indirect trauma. Fractures can be in the upper, middle and lower third of the bones of the radius, one radius, one ulna, both bones of the radius, the diaphysis of the ulna with dislocation of the radial head - Monteggia fracture (Fig. 4, a), the diaphysis of the radius with dislocation of the head ulna - Galeazzi fracture (Fig. 4, b, c). Diaphyseal fractures of the bones of P. are transverse, oblique, splintered, and crushed. Displacement of fragments in width, length, angle and rotational displacement is possible. In children, subperiosteal fractures more often occur (Fig. 5) - of the “green stick” type, when the preserved periosteum holds bone fragments and therefore their displacement is not pronounced.
As a result of trauma, epiphysiolysis can occur, which is more common in the distal radius. The degree of displacement of the epiphysis varies - from a slight asymmetric expansion of the metaepiphyseal cartilage zone to displacement of the epiphysis by half or more of the diameter of the bone. As a rule, a small bone fragment that comes off from the metaphysis is displaced along with the epiphysis (osteoepiphysiolysis).
A fracture of the distal end of the radius (a fracture in a typical location) occurs at the site of the former growth zone (2-2.5 cm from the joint space), a peripheral fragment of the radius is displaced to the dorsal side of the P.—Collis fracture (see Collis fracture); when falling on the dorsum of the hand, the peripheral fragment is displaced to the palmar side (Smith's fracture).
In case of isolated injuries to individual bones, local symptoms of a fracture are determined - local pain, disruption of the form and function of the hand and hand (see Fractures). Pay attention to the condition of the distal (in case of a fracture of the radius) and proximal (in case of a fracture of the ulna) radioulnar joints, since bone dislocation is possible. When performing radiography, pictures are taken in two projections, including the elbow and wrist joints.
For closed fractures of both bones, P. is applied for 2-2.5 months without displacement of fragments. a plaster cast in the P. position, average between pronation and supination, with flexion at the elbow joint up to 90°. In case of closed fractures of the P. with displacement of the fragments, they are repositioned (see), after which a circular plaster cast is applied (see Plaster technique). X-ray control is carried out immediately after reposition, as well as 10-14 days after it, after the cessation of tissue swelling. The period of immobilization with a plaster cast is 2.5 - 3 months. Working capacity is restored after 4-5 months. after a fracture. For isolated fractures of P.'s bones, the tactics are the same.
Osteosynthesis is used in case of unsuccessful closed reduction, secondary displacements in the plaster cast, as well as in Monteggia and Galeazzi fractures. The most common is extraosseous or intraosseous osteosynthesis of the forearm bones (see Osteosynthesis). In case of a Monteggia fracture, the dislocated head of the radial bone is reduced and temporarily fixed transosseously with a pin, and then osteosynthesis of the ulnar bone fragments is performed. For chronic dislocations of the radial head, its resection is indicated. In case of a Galeazzi fracture, osteosynthesis of the radius is performed with a plate, and the dislocation of the head of the ulna is reduced. After osteosynthesis for 2.5-3 months. apply a circular plaster bandage. When P.'s bones are fractured, a serious complication may develop—Volkmann's contracture (see Contracture).
Open fractures of P.'s bones occur as a result of direct trauma from the outside (often splintered and crushed fractures), as well as as a result of puncture of soft tissues and skin from the inside by the sharp ends of fragments.
In the case of open fractures of the bones of the P. without displacement of the fragments, as well as after successful reposition of the fragments, a cut circular or splint plaster cast is applied. Submersible osteosynthesis with metal structures can be carried out during surgical treatment of a wound with a small area of soft tissue damage, in the absence of signs of infectious complications and if it is possible to apply a suture to the wound. In case of comminuted and comminuted fractures, as well as in case of extensive wounds of P., it is more appropriate to fix the fragments with devices for transosseous fixation (see Distraction-compression devices).
In the treatment of fractures of the Forearm bones, in addition to immobilization of fragments, therapeutic exercises play a large role. This is due to the fact that the consequences of P. injuries, especially bone fractures, negatively affect the function of the hand. After applying a plaster cast on the 2-3rd day, movements begin in the joints of the hand free from the plaster cast. Perform various movements with the fingers (flexion and extension, abduction and adduction, opposition), movements along all axes of the shoulder joint. For the muscles under the cast, exercises are used that include static tension followed by relaxation. After stopping immobilization of the injured arm in its original position on the table surface, the patient performs exercises for the fingers, movements in the wrist joint, pronation and supination of the arm, and movements in the elbow joint. Exercises in warm water in the form of active movements with the brush and fingers give a good effect. For long-term swelling of the hand, a light massage of the forearm is indicated. At the end of treatment, rubber bandages, dumbbells, and expanders are used to further increase the range of motion in the joints and strengthen the muscles of the arm. To speed up the recovery of working capacity, occupational therapy is widely used (screwing in bolts with a screwdriver, working with a plane and saw, winding threads on a ball, gluing envelopes, etc.).
Rice. 6. X-ray of the forearm bones (in a Kramer splint) with a gunshot comminuted fracture: the arrow indicates a metal fragment.
Features of combat injuries, staged treatment. When using modern types of weapons, gunshot wounds to the body, damage caused by a shock wave (closed and open bone fractures, compression, etc.), as well as combined injuries, can be observed. P.'s injuries are classified according to the type of wounding projectile, the nature and location of the wound, the type of fracture, the degree of destruction of soft tissue, as well as concomitant injuries. Gunshot fractures of P.'s bones during the Great Patriotic War accounted for 36.7% of gunshot fractures of long tubular bones. Vascular injuries accompanying P.'s fractures occurred in 7.4%, and nerve damage in 30.5% of the wounded. P.'s wounds from small-caliber bullets with a high initial flight speed are accompanied by extensive destruction of soft tissue in the area of the exit hole, comminuted bone fractures, often with a bone tissue defect (Fig. 6).
When diagnosing P.’s fractures, the following are taken into account: P.’s deformation, the location of the inlet and outlet openings and the direction of the wound channel, the presence of bone fragments visible in the wound, patol. mobility at the level of the wound, pain in the fracture area, limitation of active and passive movements of the hand and fingers. The final diagnosis is established after rentgenol, research.
First aid: stopping bleeding using a pressure bandage or tourniquet, applying an aseptic bandage, immobilizing P. using improvised means, administering analgesics.
First aid: monitoring and correction of applied bandages, splints and hemostatic tourniquets, administration of analgesics, and, if indicated, improvement of immobilization using wire or plywood splints.
First medical aid: correction or replacement of bandages, splints and hemostatic tourniquets, temporary stop of bleeding - ligation of the damaged vessel or clamping it in the wound with a hemostatic clamp, administration of analgesics, antibiotics, anti-tetanus serum and tetanus toxoid.
Qualified medical care is usually provided for emergency indications (continuing bleeding, avulsion and crushing of a limb, anaerobic infection).
Specialized medical care: surgical treatment of the wound and reliable immobilization of fragments with a plaster cast; according to indications, during surgical treatment, economical resection of fragments of crushed and splintered fractures of the bones of the P. in order to ensure reliable fixation of fragments with metal structures.
Diseases
. Myositis develops after various inflammatory processes and infectious diseases (influenza, tonsillitis, abscesses, phlegmon, etc.). It may also be caused by systematic overstrain of the P. muscles, causing them to become overworked. Myositis is manifested by persistent pain, muscle weakness and impaired hand function. Treatment - rest, novocaine blockades, thermal procedures, superficial massage. In cases of persistent myositis, P. immobilization is used (see Myositis).
Aseptic tendovaginitis of the P. tendons can occur during heavy physical labor. More often, this process affects the extensor digitorum and extensor carpi radialis and ulnaris. Treatment is two or three times irrigation of the skin with chloroethyl along the affected tendon with an interval of 2-3 days; peace and warmth. Acute purulent tendovaginitis of the flexors of the fingers, which is usually a complication of felon (see), may be accompanied by purulent melting of tissues and a breakthrough of pus into Pirogov’s space. Treatment is surgical (see Tenosynovitis).
Osteomyelitis can be hematogenous and post-traumatic (as a complication of gunshot or open non-gunshot fractures) or postoperative. Hematogenous osteomyelitis of P. bones occurs less frequently than other skeletal bones. The metaphyseal part of the bones is most often affected, less often the diaphyseal. Treatment is carried out according to the principles adopted for the treatment of osteomyelitis (see Osteomyelitis, treatment).
Tuberculosis usually occurs with damage to the epiphyseal and metaphyseal parts of the bones of P. (see Extrapulmonary tuberculosis).
Syphilitic osteoperiostitis of P. bones is often asymmetrical, with focal parietal patterns. These wedges are of great importance in recognition. paintings and lab. research. Specific treatment (see Syphilis).
Mycoses (actinomycosis, spirotrichosis, aspergillosis, etc.) extremely rarely affect P.’s bones (see Mycoses).
In the bones of the Forearm, changes can be observed in hyperparathyroidism, Paget's disease, localized cysts and osteoblastoclastoma occur (see Bone cyst, Osteoblastoclastoma, Parathyroid osteodystrophy, Paget's disease).
After injuries and various diseases of the muscles and tendons of the P., as well as after fractures of the bones of the P., contractures of the hand and fingers, rotational contracture of the P., and a special form of contracture - Volkmann's (see Contracture) may occur. The complete absence of rotation of the P. can be caused, in addition to pathology of the elbow joint (see) or wrist joint (see), also by post-traumatic radioulnar synostosis (see).
Tumors
. Benign tumors. In the soft tissues of P., angioma (see), lipoma (see), fibroma (see Fibroma), lymphangioma (see), in the bones - chondroblastoma (see), chondromyxoid fibroma, chondroma (see), can develop. osteoblastoclastoma (see), osteoma (see), osteoid-osteoma (see), etc. Surgical treatment - radical removal of the lesion followed by bone auto- or alloplasty of the defect.
Malignant tumors. P.'s soft tissues can be a source of development of rhabdomyosarcoma (see) and fibrosarcoma (see). Ewing's sarcoma (see Ewing's tumor), chondrosarcoma (see), myeloma, bone reticulosarcoma (see Primary bone reticulosarcoma) in the P. area, as well as metastases of malignant tumors are rarely observed. Treatment is usually surgery followed by radiation therapy. In the early stages, saving operations are possible—wide resections of the P. bones with bone alloplasty. In later stages, amputation at the shoulder level is indicated. The prognosis for life is determined by the timeliness of treatment; with savings operations, P.'s function is largely restored.
The structure of the radius
If the ulna is located medially, the radial third is not adducted: it is located on the inside of the arm, that is, located distally. For example, the left forearm (where the ulna is on the left) contains a radius on the right. In other words, the radius is on the thumb side.
The third side of the beam is called the side, it faces outward. The superior epiphysis consists of a head with a small depression in the center for connection with the condyle of the humerus. The distal pineal gland externally contains the ulnar notch for connection with the head of the ulna.
Connection of the bones of the forearm
An important role in the anatomy of the tubular bones of the forearm is played by the way they are connected to each other. The joints allow the radius to move around the ulna. The bone can move inward or outward, with the wrist and elbow joints always working together.
When moving, the radius describes an arc of 140 degrees to the ulna. In this case, the arm and shoulder are adducted, albeit with minor movement, for a total of 220 to 360 degrees of range of motion. It is the possibility of such rotation that allows a person to perform various movements with the upper limbs.
An important place in the connection of the bones of the forearm is occupied by the interosseous membrane, consisting of collagen fibers. It lies between the radial and ulnar crests and holds them in such a way as not to restrict movement.
FAQ
In what cases does pain radiate to the shoulder?
With cervicothoracic osteochondrosis, it begins in the neck and extends to the shoulder girdle and arm.
Why might shoulder pain occur during pregnancy?
As a woman's body prepares for childbirth, the ligaments and tendons relax. This happens not only in the pelvic area, through which the fetus passes during childbirth, but throughout the entire body. This includes the shoulder joint becoming slightly unbalanced. With light loads, it may become sore. This is not dangerous.
With adequate conservative therapy, the patient can be relieved of pain, achieving complete recovery or stable remission. In medicine they know how to do this.
Literature:
- Belyaev A.S. Principles of treatment of myofascial pain syndromes / A.S. Belyaev, O.M. Maslova, I.V. Eliseeva // Manual medicine. 1994. No. 7. pp. 24-25.
- Mironov S.P. et al. Shoulder pain syndrome: monograph. Volgograd: VolgMU Publishing House, 2006. 287 p.
- Campbell CC, Koris MJ Etiologies of shoulder pain in cervical spinal cord injury. Clin-Orthot. 1996. 322(2). 140-145.
Sign up for a free initial appointment
Shoulder and forearm
The popular understanding of shoulder position creates confusion when starting to study human anatomy. What everyone is accustomed to thinking of as a shoulder is called in medicine the shoulder girdle or shoulder girdle. So where is the shoulder and where is the forearm? The shoulder is the section of the upper limb from the shoulder to the elbow joint, through which the humerus bone is connected to the bones of the forearm.
The shoulder connects to the radius from the lateral part of the articular surface, which is shaped like a ball. This is the head of the condyle of the humerus. The shoulder connects to the ulna from the medial part, forming the humerus trochlea. The coronoid and olecranon processes enter the trochlea anteriorly and posteriorly, respectively. Above the block there are pits into which the processes enter when the elbow flexes or extends.
Shoulder Pain Treatment
Treatment of shoulder pain should be carried out strictly individually, taking into account examination data and the established diagnosis. It is performed by an orthopedist-traumatologist or rheumatologist. In case of very severe pain, pain therapy is carried out by an anesthesiologist-resuscitator. A specialist will always find something to treat even very severe shoulder pain.
Diagnostics
A correct diagnosis is the path to prescribing adequate treatment and relieving the patient of pain. In diagnosis, examination and clinical examination of the patient by the attending physician using special assessment tests is of particular importance. They allow you to preliminarily determine which structures were damaged. The location of the damage is determined in more detail using functional tests.
Clinical data are confirmed by laboratory and instrumental studies that reveal inflammatory reactions, the presence or absence of infectious, autoallergic processes, the degree of destruction of articular and periarticular tissues. In identifying tendonitis and capsulitis, the main instrumental diagnostic methods are ultrasound and MRI.
How to treat shoulder pain
Treatment for shoulder pain begins with limiting the load on the affected limb. The patient is allowed movements that he can perform painlessly. Immobilization of the limb (scarf bandage) is carried out in short courses if the severity of the pain syndrome is very great. Prolonged immobilization contributes to the consolidation of hand dysfunction. Today, for partial gentle immobilization, taping is often used - fixing muscles with adhesive tapes in a certain position to prevent injury. This significantly improves the quality of conservative therapy.
After acute pain in the shoulder has been eliminated, treatment is continued by prescribing courses of physical therapy (physical therapy) and massage. At any stage of the disease, conservative therapy includes physiotherapy and reflexology courses. In case of severe pain, this is electrophoresis with novocaine, then warming procedures, mud and baths.
At the same time, drug therapy is prescribed. We remove pain by prescribing drugs from the NSAID group in tablets, injections, ointments (the drug with the best analgesic properties is Ketorol). For very severe shoulder pain, treatment includes narcotic painkillers (Tramadol) and glucocorticosteroids (GCS - Betamethosone). Sometimes folk remedies are also used.
To restore cartilage, chondroprotectors (Dona, Artra, Structum) are prescribed. Drugs in this group also help restore damaged periarticular tissues - tendons and ligaments, since they have the same origin as cartilage cells.
Surgical assistance will be required for some types of fractures, dislocations, ruptures of tendons and ligaments. If joint function is completely lost, if conservative treatment does not help, the destroyed joint must be removed and replaced with an artificial one (endoprosthesis surgery).
To prevent pain from reoccurring, a complex of rehabilitation measures is carried out using exercise therapy, massage, reflexology courses, and sanatorium-resort treatment.
What injections to give for shoulder pain
Injections are prescribed for severe pain that is not relieved by pills and external means:
- Analgin (Baralgin)
- one ampoule contains 1 ml of solution or 500 mg of active substance - a single dose for an adult; may have a toxic effect on hematopoiesis, so use it with caution; - Ketorolac (Ketorol)
– in one ampoule 30 mg of active ingredient – a single dose for an adult; contraindications: peptic ulcer of the stomach and duodenum, increased bleeding.
Blockades are widely used - injections of painkiller solutions into the most painful points.
The Moscow Paramita clinic uses the most modern methods of diagnosis, treatment and rehabilitation of all diseases that cause shoulder pain syndrome.
If necessary, if the disease threatens the patient’s life, after examination by a doctor, he is urgently sent to the hospital. But we treat most pain syndromes on an outpatient basis. Detailed information about treatment can be found on our website.
Injections for shoulder pain
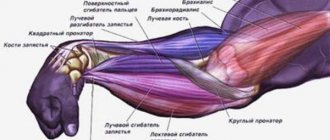
Forearm muscles
We have already figured out where a person’s forearm is. Let's take a closer look at which muscles are involved in this segment of the upper limb. Depending on the movements performed, the muscles of the forearm can be divided into:
- instep supports: allow the beam to move outward;
- flexors and extensors of the fingers.
- pronators - ensure the movement of the beam inward;
- flexors and extensors of the hand;
These muscle groups are divided into two main categories based on their location: anterior and posterior.
Anterior forearm muscles
The anterior muscles that move the forearm are where the radius points inward. The group also includes flexor muscles. The superficial layer of muscle tissue of the anterior muscles begins from the medial part of the epicondyle of the shoulder. The deep muscle layers begin from the bones of the forearm and the mesh between them. The pronators are attached to the radius.
The muscle tissue closest to the humerus is more pronounced and closer to the structure of the wrist and consists mainly of tendons.
The superficial layer of the anterior muscles consists of:
- Pronator teres: participates in forearm flexion and also promotes inward rotation (palm downward).
- Brachioradialis - participates in the process of supination and pronation, in flexion of the forearm. It originates in the humerus and inserts into the distal radius.
- Radial wrist flexion: Involved in flexion of the arm and partially internally rotates it.
- Palmaris longus muscle - flexes the arm.
- Flexor carpi: Involved in the movement and flexion of the arm.
- Flexor digitorum superficialis: involved in flexion of the middle phalanges of the fingers.
The deep layer of the anterior muscles is represented by the flexor pollicis longus, flexor digitorum profundus and pronator quadratus muscles. The forearm, where many of the muscles involved in the movement of the upper limb are involved, determines the dexterity and variety of actions performed.
How to prevent shoulder pain
To prevent pain from occurring, the following conditions must be observed:
- lead an active lifestyle, move more, engage in feasible sports;
- Avoid prolonged periods with your arms raised above your head, as well as movements associated with unilateral load on the shoulder joint; At risk are weightlifters, tennis players, and miners; If a representative of one of these groups feels persistent pain in the shoulder, perhaps he should change his occupation or at least reduce his exposure to harmful factors as much as possible.
Posterior muscles of the forearm
The posterior group of muscles of the forearm consists of the supports and extensors of the instep. The superficial layer of muscle tissue consists of muscles:
- Extensor carpi radialis longus: involved in flexion of the forearm at the elbow and extension of the wrist.
- Extensor carpi radialis brevis - participates in wrist extension and abduction.
- Extensor finger.
- Extensor of the little finger.
- Elbow extensor wrist - participates in abduction of the wrist to the elbow and its extension.
The deep layer of the posterior muscles of the forearm is represented by the support of the instep, the long muscle (involved in abduction of the big toe), the short and long extensor of the pollicis and the extensor of the index finger.
Nerves of the forearm
The forearm, where many muscles are located, is also where nerves pass. Let's take a look at the main nerves located in this area and their functions:
- Median: branches are located in the elbow joint and the anterior muscles of the forearm. It innervates the joints of the hand and the muscles of the thumb.
- Medial cutaneous - innervates the skin of the forearm, originating from the medial bundle.
- Musculocutaneous - its branches are located in the elbow joint, descending below it in the form of the lateral cutaneous nerve. Innervates the skin of the forearm.
- Radial: The deep branch of this nerve innervates the extensor muscles of the forearm.
- Ulnar - located near the ulnar artery, innervates the flexor carpi ulnaris. Below it is divided into branches that innervate the palm from the inside and outside.
Fractures of the forearm bones
The bones of the forearm are quite thin, so they break easily even with minor injuries.
Forearm fractures can be divided into several types:
- Fracture of the elbow joint - occurs due to a fall on the elbow or due to a strong contraction of the triceps. It is characterized by swelling with a bluish tint, sharp pain when moving, deformation or drooping of the arm.
- Damage to the coronoid process - occurs due to a fall on a bent elbow. Complaints of swelling, limited movement and pain.
- Fracture of the proximal bone - caused by a fall on the elbow in a bent position.
- Fracture of the ulna or radius - occurs due to a direct blow. The main symptoms are swelling, severe pain and limited mobility.
- Fracture of both bones of the forearm - characterized by displacement of the broken bones and their convergence.
In case of fractures, it is extremely important to provide first aid to the victim. If the fracture is open, you should not try to fix it yourself. It must be remembered that two joints are necessarily immobilized: the wrist and the elbow. To do this, you can apply a splint without touching the side of the arm from which the bone protrudes.
The forearm is an important segment of the upper limb, providing high mobility of the hand and a variety of actions performed.
Rehabilitation after osteosynthesis surgery of the middle third of the forearm.
After osteosynthesis surgery, it will take a short period of time for swelling and pain to subside before you begin active rehabilitation. In the early postoperative period, it is possible to use a scarf bandage to reduce pain and for disciplinary purposes. Topical use of ice or cryotherapy gel bags, which are sold at any pharmacy, can effectively combat pain and swelling. Their use is also possible at a later date from the operation.
For the first 2-3 weeks, physical therapy is limited to performing movements in adjacent joints - the elbow and wrist; starting from the 3rd week, a gradual onset of rotational movements is possible. Full amplitude is restored by 6 weeks after the intervention. Physical activity is not allowed before there is a clear x-ray picture of fusion, which usually occurs by 3 months. The decision to remove metal fixators is made no earlier than 2 years from the date of surgery.