Active running training is not without injuries. Pinching of the soleus muscle, which is located on the lower leg, is also possible. Aching pain occurs.
Playing sports will only be beneficial if a person studies his body and learns to listen to it. But, if you still cannot avoid muscle injury, it is important to make a decision on the correct treatment, which the attending physician will tell you about.
The triceps surae muscle is formed from the gastrocnemius and soleus muscles. It is this connection that controls the foot, sets it in motion, and bends the sole in the desired direction. It plays a big role in performing jumps and various types of running, and serves as a muscle venous pump.
Functions
Thanks to the triceps muscle, the human foot extends in the plantar direction. With the help of the plantar, long and short peroneal, tibialis posterior, muscles flex the foot at the ankle joint when the knee is extended, and if the knee is bent, the sole is flexed only by the soleus muscle.
This organ stabilizes the knee joint under postural, static and dynamic loads. Participates in the minor work of flexion of the knee joint, covering the grace and sartorius muscles, which counteract the quadriceps. The main work is shown in running, cycling, jumping and squatting.
Soleus muscle. Where is
There are 2 functions:
- when a person jumps, the legs bend at the knees and the push is made by the toes, after which the legs straighten - this is where the organ is involved;
- when straightening the legs, the gastrocnemius muscle begins to participate, therefore the direct responsibility of the soleus muscle is to distribute and withstand the load with straight legs.
When the soleus muscle contracts, it compresses the small veins, causing blood to flow back to the heart. The way blood flow works is that small valves resist the pull of gravity, allowing blood to flow towards the heart.
Therefore, the process of returning blood is directly related to the expulsion of blood by the soleus muscle - because of this unique process, it is called the “second heart”.
Anatomy
Friends, on June 14-15 in Moscow there will be a seminar by Yuri Sdobnikov “Analysis of running, diagnosis of disorders. Prevention and treatment of lower extremity injuries.” Find out more...
Start and Attachment
- The muscle starts from the posterior surface of the head and the upper 1/3 of the body of the fibula, as well as the middle 1/3 of the tibia, the interosseous membrane of the leg, which is located between the tibia and fibula.
- The soleus muscle is attached to the heel bone (together with the gastrocnemius muscle) through the Achilles tendon.
Function
- Plantar flexion of the foot at the ankle joint.
- When you stand, the heel bone becomes the fixed origin of the muscle and maintains the upright position of the body.
- The soleus muscle stabilizes the tibia relative to the calcaneus, limiting forward motion.
Innervation
- Tibial nerve L4, L5, S1, S2.
Structure
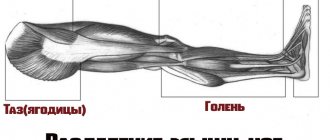
The soleus muscle is located on the back of the lower leg under the calf “heads”. A muscle can be called one large bundle of fiber, which has a flattened shape.
The attachment is the Achilles tendon, which is in contact with the calcaneal tubercle and supplies blood to the calf arteries.
Types of diseases
Pain in the soleus muscle is a universal symptom that can occur in different diseases. Since the blood supply originates from the popliteal arteries, endothelial cavities (sural sinus) are formed in the thickness of the muscles.
| Stenosolia | A disease that is characterized by narrowing, squeezing pain in the red muscle, lasting more than a minute. Covers one part of the middle section from the outer or inner side of the fibula. It manifests itself as excruciating pain with burning and numbness. If you palpate the edges of the muscle along the lateral and medal heads, you can determine the hypertonicity of the area. |
| Polymyositis | An autoimmune disease of the soleus muscle, which manifests itself as intoxication and dull pain when moving. The muscle becomes swollen and painful on palpation, after a while nodules, fibrosis, and calcifications are felt. |
| Myositis | Oncological, parasitic disease, complicated by a cold, injury or overexertion. |
| Fibromyalgia | A disease of autoimmune origin, manifested by intense constant pain, severe weakness in the soleus muscle, which is in daily morning stiffness. |
| Crumpy | A brief, localized, painful cramp that squeezes and tightens a muscle. Muscle contraction occurs slowly and lasts from 1 second to 1 minute. The reason lies in the disruption of the nutrition of nerve endings. Cramps occur at night or after strenuous exercise. |
| Calf muscle rupture | The symptom of a rupture is almost impossible to distinguish from overvoltage. If the cause of the pain is not identified in time and periodic exercise is given, the muscle may tear. It manifests itself as a sharp and acute pain, the presence of something burst or torn. |
Symptoms
The pathology of the anatomical organ is manifested by symptoms such as fainting or swelling of the legs.
Pathological changes in painful sensations manifest themselves in the following areas:
- back of calves;
- heels and soles;
- lower back and sacrum;
- foot joints;
The pain mainly radiates to the heel area. A person may experience sleep disturbances and restrictions in movement, lameness, difficulty walking, aching pain at night, and increased tension.
The flexion function becomes limited, and there is blunted mobility of the toes. If movement restrictions continue, inflammation of other parts of the body may occur. The work of the soleus muscle can be replaced by trunk muscle structures. Can occur when climbing a mountain, from a chair, bending toward the floor, or going down stairs. Symptoms vary for a number of reasons.
Pain while moving
The symptom is a sharp flash of pain in the leg or aching pain in the back, discomfort in the buttock. This condition is provoked by prolonged immobility or sitting, physical activity, and stress.
Pain due to injury
Appears when a rupture occurs - complete or partial. The symptom is a swollen, painful area. The tear can be located anywhere in the soleus muscle.
A person may not feel a stretch of the soleus muscle, but pain and swelling will appear after a few hours. The main thing is to be able to distinguish a rupture of the soleus muscle from other injuries, which is located in the back of the lower leg.
Clinical symptoms of the soleus muscle show a protective reaction of the body. Pain signals that the limb needs to be protected from further stress. Microtear of the fiber is provoked by the development of inflammation and swelling of the soft tissues.
Damage to the soleus muscle is divided into 3 degrees:
- I degree – manifests itself as a slight stretch in the muscle fiber. Has moderate pain that appears some time after injury. There may be swelling, deviations in the movements of the limbs with increased pain or tension.
- ІІ degree – part of the fiber is torn. There is acute pain and swelling of the lower leg. Possible hematomas. The muscle hurts when moving.
- Grade III – the muscle is completely torn and disconnected from the Achilles tendon. Pathological mobility of the ankle appears. It is characterized by painful shock and the formation of an extensive hematoma. When symptoms first appear during an injury, a muscle tear may be suspected.
Pathology
Accessory soleus muscle (ASM)
DCM is present in 0.7-5.5% of people and usually makes itself known in the second or third decade of life. It is more common in women (the ratio between women and men is 2:1).
The DCM is located under the gastrocnemius muscle. The muscle originates at the level of the posterior upper third of the fibula (sometimes between the head of the fibula and the posterior part of the body of the tibia). From its origin, the DCM passes medially until it reaches the Achilles tendon.
There are several different options for attaching DCM:
- Achilles tendon.
- Upper part of the heel bone.
- Medial part of the calcaneus.
The clinical picture of DCM is characterized by pain during exercise. However, if the patient is asymptomatic, no therapy is required. If pain or other discomfort is caused by exercise (and we associate this with DCM), exploration with fasciotomy or excision of the DCM is recommended (as in some cases it is not possible to determine the origin and insertion of the DCM even with MRI).
Stretching and tearing
A complete or partial tear (most commonly) of the soleus muscle occurs when the muscle is stretched during its contraction (eccentric contraction). The rupture in many cases occurs where the soleus muscle attaches to the Achilles tendon, causing inflammation.
The clinical picture is characterized by pain when activating the triceps surae muscle (walking on toes, running, jumping), when pressing on the Achilles tendon 4 cm above the heel bone and stretching it.
In all cases where there is a sensation of “tearing” or sudden shooting pain in the Achilles tendon, you should seek medical help as soon as possible. For diagnosis it is better to use ultrasound or magnetic resonance imaging.
Whenever the triceps surae muscle is strained/injured and the soleus muscle is affected, then medial or lateral pain occurs i.e. pain along the fibers. When the calf muscle is affected, the pain is localized in the center of the triceps muscle. However, most often both muscles are affected at the same time.
Causes of organ diseases.
The soleus muscle is in the stage of movement when the ankle joint extends and the muscle venous pump functions.
- Pain occurs during physical activity. If a person has untrained muscles, his legs will hurt after running. This happens because the tissues accumulate lactic acid during heavy exercise, without having time to be eliminated properly, and the human body, in turn, begins to experience pain.
- Pain may occur when standing motionless or tense for a long time. For example, on an airplane, at your desk, walking on your toes. The blood begins to stagnate, the muscle pump stops working, and because of this, blood stops flowing from the legs to the heart. The arteries accumulate endotoxins, circulation and oxygen supply are disrupted - all this leads to severe pain. You can correct everything by raising your legs to the level of your heart and holding them in this position for 15-30 minutes.
- If a person works in the same position and the ego cannot be changed, varicose veins of the limbs form. This disease can be prevented only with the use of daily prevention. You can do light exercise or, if possible, elevate your legs on a pillow.
- Flat feet also cause pain in the soleus muscle. The shape of the feet changes with age, and walking becomes difficult, pain appears up to the knee area. To solve this problem, physical therapy is used and specialized shoes for flat feet are worn. But first you need to visit a doctor.
- The human body has many parasites, and those that are harmful to health can become colonized. These include trisinellosis larvae. Due to their penetration into muscle tissue, severe pain, allergies and fever are felt.
- Nerves have a strong influence on the well-being of the legs. When the sciatic nerve is inflamed, pain is felt in the buttocks, which then goes down. The reasons for this phenomenon are varied, but doctors are inclined to diabetes mellitus.
- Cramps are not a rare cause of muscle pain. Contractions and sharp pain occur. This happens if the body is dehydrated and not filled with magnesium, potassium, and calcium.
- Any disease of the spine also leads to muscle pain, which begins in the lower extremities, but there is no pain in the vertebrae. Excess weight, in turn, affects the health of the spine and legs. Therefore, all diseases are interconnected, regardless of age.
- Cellulite inflammation with ulcers mainly causes pain in the legs. When the skin is damaged, pathogenic microorganisms penetrate the cells. Therefore, this can lead to severe pain, high fever, and weakness.
Soleus muscle
It is in the summer that clients most often come with complaints of pain in the soleus muscle. Even the slightest injury to this muscle leads to severe and prolonged pain and, most often, runners suffer from such injuries. Especially those running on hilly terrain.
The soleus muscle (Fig. 1) is the largest and strongest muscle of the lower leg. It is so strong due to its complex structure. The soleus muscle is attached from above to the head and upper third of the body of the fibula along its posterior surface, as well as to the line of the soleus muscle of the tibia, and from below the muscle is attached to the calcaneal tubercle by the Achilles tendon. It lies inside the calf muscle. These two muscles are closely related, with some of their fibers running parallel. Some consider the two muscles to be the same structure, but their functions are different and tests specific to each muscle are needed to determine whether injuries are present.
Pain in the soleus muscle can be felt as pain deep in the lower leg, at the top of the knee. Discomfort can be felt at a specific point or spread to an area, since in some cases a whole group of muscle fibers can become inflamed and the reason for this is the extremely large length of a given muscle.
Main causes of damage
It takes a lot of tension to injure this muscle. As mentioned earlier, the soleus muscle receives the greatest tension when running uphill, because during such a run a person has to bend his knees more than usual. The muscle receives the same tension when jumping high. Most people do not know how to land correctly by “rolling” on their feet and simply land on their toes with their knees bent. Over time, the muscle wears out and eventually becomes injured.
Posture and gait also affect the condition of the soleus muscle. For example, if a client has a pronated foot when walking and also has flat feet, the pressure of most of the body weight falls on the medial part of the foot. This, in turn, shifts body weight pressure from the lateral to the medial portion of the soleus muscle, causing one part of the muscle to receive more load than the other and therefore creating an imbalance in muscle fiber development. Consequently, when the force is physiologically directed to the medial part of the muscle, all parts of the muscle are susceptible to injury - the medial part due to excessive load, and the lateral part due to its weakness.
The head and neck can also “contribute” to injury to the soleus muscle. If the head is moved forward excessively when walking, the back of the lower leg acts as a compensator and receives additional load. Prolonged overuse of the back of the legs puts them at increased risk of injury and various musculoskeletal conditions.
How to Determine the Presence of an Injury
When the soleus muscle is injured, a person feels a dull, aching pain during or immediately after physical activity. The pain is often rated as tolerable, but many people have to give up sports such as tennis, cycling, or running because of it. As the disease progresses, the pain can become so intense that it becomes difficult for people to even walk. We offer three tests to help determine if a soleus muscle injury is the true cause of your pain.
Calf raises with bent knees
Ask the client to stand with their bare feet on the floor, feet shoulder-width apart, feet parallel to each other. Next, the client should bend their knees as much as possible, placing their heels firmly on the floor and keeping their back straight. Ask him to rise up on the balls of his feet several times, keeping his knees bent and lifting his heels as high as possible. If the soleus muscle is injured, it will cause discomfort or pain.
Single leg calf raise with bent knees
If the first test does not reveal any symptoms of injury, try the next variation, which increases the load on the injured area. Ask the client to stand on one leg (the one with pain) while holding onto something for balance. Next, the client should rise onto his toes with his knee bent, lifting his heel off the floor to the maximum possible height. As stated earlier, the soleus muscle is very strong, and this test alone may not detect pain, especially if the client experiences pain after a five-mile run or a half-hour game of tennis. If there is no pain during the test, repeat the test immediately after performing any activity that usually causes pain, in which case the test should increase the pain or discomfort many times over. If the test did not show anything in this case, most likely the cause of the pain in this case is an injury to the calf muscle.
Foot position test
Ask the client to stand in a familiar position and carefully assess the position of his feet. Ideally, they should be parallel or turned outward by a maximum of 5 degrees. If the feet are turned laterally by 10-20 degrees, their arches can practically touch the floor. If the client bends his knees 5-6 cm forward, with his feet turned outward, the knees will point straight.
To relieve stress on the medial leg and prevent injury, the client must develop the habit of standing correctly. Treatment for the soleus muscle is usually long-term: the stronger the tension, the longer the rehabilitation period.
Independent muscle training. Massage. Friction therapy
There are many ways to get rid of soleus muscle pain. For moderate injuries, it is often sufficient to perform calf raises with your knees bent and avoid excessive strain. In this case, recovery will take several months.
The main mistake is an early return to usual activity - before the muscle’s functioning is completely restored.
Friction therapy along with massage speeds up the recovery process, shortening the recovery period to 4-6 weeks in mild cases and 8-12 weeks for severe injuries.
In friction therapy, the client must lie face down on a massage table. Approaching the table from the side, bend the client's leg at the knee to 90 degrees. Place his ankle on your shoulder, keeping his knee bent at a 90-degree angle. Cup your leg with your fingertips pointing directly at the center of your calf, holding your shin with your thumb. Move your fingertips to the center of the gastrocnemius muscle to contact the soleus muscle. Applying pressure anteriorly, move horizontally, from medial to lateral, for 1-2 minutes. Then move your palms to another part of the soleus muscle, covering the entire area sequentially. After 5-6 minutes, give the client a rest and do the same again. After these frictions, do a five-minute massage of the calf muscle.
Exercises for the soleus muscle
We recommend the following exercises to all clients with soleus injuries. Their daily implementation speeds up recovery many times over.
Stretching
Start with a warm-up - walking for a couple of minutes or bending and straightening your legs while sitting. Next, sit on the floor and bend one leg at the knee at an angle of 90 degrees. The knee should be pointing towards the ceiling and the foot should be firmly on the floor. Make sure your foot is aligned with your shin (not turned in or out). First, pull the toe of your foot towards your shin using muscle force, then grab your foot with your palms and pull it towards the knee (see figure). Pull the toe for two seconds, then lower your leg to the floor. Do not pull on the sock for more than two seconds. Repeat this exercise 8-10 times with each leg.
Strengthening the soleus muscle
Stand straight and rise onto your toes with your knees bent. The feet should be parallel and shoulder-width apart. Raise your toes 3 times for 10 reps with little rest between sets. If you feel that these three approaches are easy for you, complicate the exercise - turn your feet 45 degrees inward and outward.
You can also make this exercise more difficult by standing with your toes on the edge of the step, lowering your heel below parallel with your foot. Try starting the exercise with your legs straight and gradually bending your knees as you go.
The last stage is the use of weights. You must learn to perform this exercise with a weighted device while standing on one leg while holding onto something for stability. This exercise trains not only the soleus, but also the gastrocnemius muscle, especially with bent knees. As the muscles strengthen, it will become easier and easier for the client to perform all stages of the exercise with legs bent at the knees.
Orthopedic products
In some cases, a podiatrist can help correct misaligned feet. However, this will require a lot of time and a good therapist - not everyone can afford it.
There is a simpler solution - use orthopedic products (shoes, insoles, etc.) to relieve tension from the soleus muscle caused by improper foot position. They can be purchased at pharmacies, shoe stores, or ordered online. However, to achieve the best therapeutic effect, shoes or insoles must be made to order, taking into account the individual characteristics of the foot structure.
CONCLUSION
Injuring the soleus muscle requires extremely intense impact, and recovery can take a lot of time and patience. By combining friction therapy, massage, strengthening and stretching of the muscle, you can speed up the recovery process, and correcting incorrect foot position will help avoid injury in the future.
Diagnostics
The pathology of pain in the soleus muscle is determined by clinical and instrumental studies. By contacting a doctor, he will rule out causes that pose a health hazard - thrombophlebitis, thrombosis, cancer and various infections.
Inflammation of veins and blood clots are determined by Doppler ultrasound system. Blood patency problems are determined, and transillumination will show damaged veins. The use of duplex angioscanning will show the condition of the blood clots, their age, and the state of the lumen.
If the doctor suspects that the muscles hurt due to the spine, he prescribes X-ray examinations of the hip joints and pelvic-sacral joint. Magnetic resonance imaging is also used, and a blood test will show the percentage of trace elements in the blood.
When to see a doctor
A trip to the doctor should start from the outpatient department to the therapist. First of all, he examines the patient and writes out a referral for tests and other examinations. Will formulate a pre-treatment to reduce soreness of the soleus muscle. After a comprehensive examination, the doctor will take further action.
If necessary, a narrow specialist will write out a referral, because without preliminary tests, a narrow specialist will not undertake to examine the patient, as this is pointless.
Based on the above, the following symptoms are identified that determine when to go to the doctor:
- Severe pain in one or both legs for 4 or more days.
- Numbness of the limbs, in which weakness, heat and cold are felt.
- A painful sensation that can radiate to another part of the body.
- The skin became pale and cyanotic.
- My feet are constantly freezing and swelling.
- Limited movement with tight muscles.
- Painful flexion and extension of joints.
Prevention
To avoid pain in the soleus muscle, you need to follow some rules:
- Avoid fatty foods if you have vascular problems
- Make adjustments to your weight
- Use exercises every day to strengthen your muscles.
- With a sedentary lifestyle, it is important not to forget about morning exercises.
- When training, pay attention to your body’s signals; if there is discomfort, you need to stop.
- Warm up correctly, starting to warm up your muscles with a light jog.
- After intense training, do not forget about stretching.
Medications
The soleus muscle is located between the shin bone and the gastrocnemius muscle. If the gastrocnemius muscle shortens or increases in diameter, it creates pressure on the soleus muscle, pushing it towards the tibia. Therefore, the soleus muscle becomes pinched, followed by pain and inflammation.
Depending on the severity of the injury, various measures can be taken to support the natural healing process. If pain in the soleus muscle cannot be tolerated, medications are used. For this case, there are creams and ointments based on anesthetic.
Treatment in the first three days can take the following measures:
- Decongestant ointments (eucalyptus balsam, therapeutic and sports ointment based on arnica).
- Taking anti-inflammatory drugs (Diklak-gel, Menovazin, Fastum-gel). These non-steroidal anti-inflammatory agents are applied 3 times a day using light, circular motions. Finelin and Warfarin are taken in tablet form.
- Taking medications that thin the blood (Arixtra, Zilt, Plavix).
- Taking muscle relaxants that reduce muscle tension (Pancuronium, Mivacurium, Trubocurarine).
After 7 days of pain, treatment should continue with warming ointments such as Viprosal or Ben - gay. These agents, which stimulate microcirculation in tissues, restore elasticity to the soleus muscle. An ointment based on snake venom will also help overcome pain.
Non-steroidal, anti-inflammatory drugs, groups of analgesics (Revmaxikam, Fanigan, Ibuprofen, Meloxicam) are also used internally.
A deficiency of the minerals sodium, potassium or magnesium can lead to muscle pain. Sodium and potassium are important for fluid balance and nerve and muscle function. Magnesium is also essential for nerve and muscle function and is involved in energy metabolism. However, minerals should not be taken without medical advice. Here it is necessary to do a clinical blood test in advance.
Currently, the vast majority of phlebologists recognize dysfunction of the muscular-venous “pump” of the lower leg as an important link in the pathogenesis of varicose veins of the lower extremities [1-3]. A significant role in the implementation of this mechanism is assigned to the veins located in the thickness of the largest muscles of the leg - the gastrocnemius and soleus [4-6]. Considering the complex anatomical and physiological features of the structure of the muscular veins of the leg, their numerous connections with each other, with deep and superficial veins, the study of these veins presents certain difficulties [7]. At the same time, their important role in the venous hemodynamics of the leg indicates their special importance in the accurate diagnosis of pathological changes in this part of the venous system [8], which in all cases should be based on a thorough knowledge of the anatomical structure of the entire venous line of the lower extremities.
However, not only in most manuals on ultrasound and x-ray diagnostics, but also in numerous anatomical atlases, there is no description of the architecture of the intramuscular veins of the leg [9–14]. The study previously undertaken by the authors of the features of the anatomical structure of the venous collector of the soleus muscle was based on the results of radiopaque phlebography and post-mortem dissection of the extremities, which, of course, did not allow reproducing the exact spatial location and establishing all communication connections of the intramuscular veins of the leg with each other, as well as between the deep and superficial veins [ 4, 15, 16]. For this reason, multislice computed tomography-venography (MSCT-venography) with image reconstruction in 3D mode was used as the main method for visualizing the venous bed of the lower extremities.
The purpose of the study was an intravital study of the features of the anatomical structure of the venous collector of the soleus muscle using MSCT venography.
Using the MSCT venography method for the period 2015–2018. 400 people of both sexes with chronic venous diseases were examined, who were distributed, in accordance with the international CEAP classification, as follows: C0—50 (12.5%) people, C1—58 (16.5%) people, C2—C3 - 173 (49.5%) patients and 119 (34%) individuals had trophic disorders (C4-C6).
The studies were performed on a 128-slice multislice computed tomograph Philips Ingenuity CT (Netherlands) with the Intell Space Portal image processing software package (Netherlands), followed by reconstruction of a volumetric image in 3D mode. Initially, in order to standardize the “lower” MSCT venography, we developed our own research methodology, which differs from previously used methods by clear time criteria for delaying the start of scanning from the moment of bolus administration of the radiopaque mixture, the number of consecutive scans and the stages of functional tests [17].
When systematizing the data obtained in order to classify the identified patterns of the anatomical structure of the veins of the soleus muscle, the division of veins into main, network and intermediate development variants was used (Fig. 1).
Rice. 1. Options for the development of the venous collector of the soleus muscle (diagram). Single and paired trunks with Y- and V-shaped division of the venous main into veins of the 1st, 2nd and 3rd order were identified (Fig. 2).
Rice. 2. Classification of veins of the soleus muscle (MSCT venography).
The main segments of veins from the place where the intramuscular vein flows into the deep vein to the visually determined first tributary were classified as first-order veins. From this level, the venous line received the name axial vein of the 2nd order. Veins of the 3rd order were represented by multiple and smallest vessels, which, in fact, are the beginning of the entire venous collector. These veins were considered as the main communicating anastomoses, connecting the veins of the soleus muscle with each other, with the veins of the gastrocnemius muscle, with the deep veins or the subcutaneous venous collector. In the latter case, the localization of the identified perforators corresponded to the generally accepted groups in phlebology: posterior tibial, lateral, paratibial, paraachilles and intercapitate groups.
To assess the variability of the shape of the veins, we used the classification we developed, according to which we distinguished cylindrical (regardless of the diameter of the vein, but with parallel walls of the vessel) and fusiform (spindle-shaped) forms, subdividing the latter into local and extended ectasia.
In 400 lower extremities examined, 8510 soleus veins were identified.
As a result of the studies, the venous collector of the soleus muscle was represented by single (65%), paired (18%), Y-shaped (96%) and V-shaped (13%) trunks, having a mixed appearance in 82% of cases.
The main venous trunks of the soleus muscles (soleus veins of the 1st order) were identified in 6212 (73%) cases. The length of the main trunks of the cylindrical soleus veins was subject to significant fluctuations from 2 to 8-10 cm. The veins of the soleus muscle in 70% of cases flowed into the posterior tibial vein, and in 30% into the peroneal vein. At the same time, the diameter of the venous trunks did not exceed 0.5 cm, the angle of entry of the intramuscular veins into the deep veins of the leg averaged 30°, valves were found in 100% of observations. The connections of the veins of the soleus muscle with the anterior tibial veins, as well as their drainage into the popliteal vein, were not recorded. Second-order axial veins were identified in 7063 (83%) cases. Terminal veins of the 3rd order were present in all cases and, having a large branched network, perforating the muscular fascia, rushed towards the posterior tibial veins or to the more superficially located veins of the gastrocnemius muscle (visualization in 92 and 98% of cases, respectively). Using the division of the common venous main into veins of the 1st, 2nd and 3rd orders, depending on the degree of presence of these veins, we identified the main, network and intermediate variants of the development of the veins of the soleus muscle, the characteristics of which were brought to final clarity. The main variant of development was present in 63% of cases; it was characterized by the presence of a pronounced main trunk with axial veins extending from it, ending with veins of the 3rd order, along the entire length up to the tendon part of the soleus muscle. In the network variant of development (8%), the short main trunk was identified only immediately before the venous main flows into the posterior tibial vein. In this case, most of the venous collector was represented by equivalent veins. Visually, the impression was created that in the absence of axial veins, almost all veins (except for short main trunks) could be classified as third-order veins. An intermediate variant of the development of the soleus venous line occurred in 29% of cases. In this case, the classic step-by-step formation of the axial and main veins took place at the appropriate projection level.
The depth of the intramural path of the main veins in the soleus muscle has not been precisely established. However, when analyzing in 3 planes, it could be concluded that in 72% of cases the main trunk was oriented medially from the midline of the posterior surface of the leg, which is apparently associated with a greater functional load and intensive drainage function of blood flow into this vein from the side of the great pool saphenous vein. Also on the medial (inner) side there was the largest number of perforating veins associated with the soleus veins. In 48% of cases, a clear connection was noted with the oblique vein, in 23% - with the intersaphen vein and in 57% - with the posterior arched vein, that is, they belonged to the posterior tibial group of Cockett (Fig. 3).
Rice. 3. Layer-by-layer MSCT visualization of the perforating veins of the posterior tibial group associated with the soleus venous collector.
A typical junction of the veins of the gastrocnemius and soleus muscles was the place of transition of the muscular part of the gastrocnemius muscle into the tendon muscle, which corresponded in 87% of observations to the middle third, and in 13% to the lower third of the leg. At the same time, the soleus veins of the 3rd order were connected to the gastrocnemius veins of the 3rd order in 73% of cases. In 15% of cases, a direct connection of the 3rd order gastrocnemius veins with the axial veins of the soleus muscle was noted. Direct connection of the soleus venous collector with the main trunk of the small saphenous vein was noted in 63% of cases through perforators of the paraachillary group (Fig. 4),
Rice. 4. Muscular perforators of the venous collector of the soleus muscle. in 8% of cases - through the perforators of the intercapital group, and in 47% of cases - through the perforators of the lateral group (Fig. 5).
Rice. 5. Layer-by-layer MSCT visualization of the perforating veins of the lateral group associated with the soleus venous collector.
Analysis of the variability of the shape of the veins of the soleus muscle showed that of the total number of patients examined, the cylindrical shape of the veins was present in 35.9% of cases, and in 64.1% of cases the veins had fusiform ectasia of varying length. The percentage of the presence of veins of the indicated forms, as well as the number of detected ectasia, depending on the extent, was different and changed from the group of patients C0-C1 to C4-C6. Thus, if among patients with class C0-C1 in 83.1% of cases the veins had a cylindrical shape and only 16.9% of patients had fusiform local ectasia, then in patients C4-C6 a cylindrical shape was noted only in 11.6% observations, and 88.4% of patients, that is, the majority, had fusiform ectasia, which in almost half of the cases was extended (Fig. 6).
Rice. 6. Changes in the shape of the veins of the soleus muscle with the development of their ectasia.
The first and still most significant works on studying the capabilities of MSCT venography in studying the features of the anatomical structure of the veins of the lower extremities were studies conducted by the French vascular surgeon and anatomist J.F. Ulem, as a result of which it was concluded that a new method for studying the venous system of the lower extremities is promising [18—20]. The research carried out by J.F. received special recognition throughout the world. Ulem in recent years has studied, using MSCT venography, the functional anatomy of the ankle musculovenous pump from the point of view of participation in the venous outflow from the lower extremities of the perforating veins of the leg and foot [21]. However, the venous collector, directly located in the thickness of the soleus muscle, was not described by this author.
The ambiguity of many details of the structure of the soleus veins, despite their significant significance in the physiology of venous return from the lower extremities, served as the basis for a special study of this issue.
As a result of the studies, the first important conclusion was made that the venous collector of the soleus muscle is, on the one hand, an independent structural unit, and on the other hand, it is extremely well integrated into the general venous circulation system of the leg, being, in fact, a powerful intermediate drainage link between the superficial and deep veins from the point of view of the functioning of the muscular-venous pump of the leg as a whole.
The need to separately consider the venous collectors of the gastrocnemius and soleus muscles is due to differences not only in their anatomical structure, but also in their functional purpose. Thus, the soleus muscle has a long, fusiform shape and is involved in flexion of the foot. However, based on a comparative analysis of the points of fixation of the soleus muscle and the deep muscles of the leg, it should be noted that there is a predominant static load on the former and a dynamic load on the latter. The gastrocnemius muscle is a typical biceps muscle; its main purpose is to actively and powerfully flex the lower leg. It is natural that the degree of participation of these muscles and their venous collectors in the unified functioning of the muscular-venous “pump” of the lower leg will be different and far from unambiguous.
The venous collector of the soleus muscle begins to form by the fusion of small branches of the 3rd order in the lower or middle thirds of the leg, which are subfascial segments of indirect perforating veins, belonging in 57% of cases to the posterior tibial group, as well as to the paraachillary and lateral groups in 63 and 47 % respectively. In these cases, the vascular network is represented by paired veins of equal diameter or one larger trunk and a thin paired vein. In 73% of cases, through third-order veins, a communication connection of the soleus venous collector with the veins of the gastrocnemius muscle in the projection of its medial and lateral heads was noted. There was no direct connection of the saphenous veins with the veins of the soleus muscle in the upper third of the leg, bypassing the venous collector of the gastrocnemius muscle. In the middle and lower thirds of the leg, the connection of the veins of the soleus muscle with the subcutaneous venous lines is common, and this happens, as noted above, in 57% of cases in the basin of the great saphenous vein through perforators of the posterior tibial group, and in 55% of cases - in the basin of the small saphenous vein through perforators of the paraachillary and lateral groups. Axial veins of the 2nd order are formed from veins of the 3rd order and are represented by single or paired trunks, which, before flowing into the posterior tibial vein, are combined into 1 or 2 main trunks, the length of which can be different.
Studies have shown that the previously expressed opinion that the formation of the venous collector of the soleus muscle is possible according to the type of open hemodynamic arches [4, 7, 22] is inaccurate. Having traced the course of the main venous highways of the soleus muscle in 3D mode in 3 planes, we observed the intramuscular venous collector along its entire length and concluded that the hemodynamic arches were closed in 97.3% of observations. This clarification made it possible to conclude that the intramuscular veins of the leg are not simply auxiliary tributaries of the deep veins, the main purpose of which is to ensure outflow from the muscle mass of the leg, but play an important role as a drainage mechanism, the functioning of which, from a hemodynamic point of view, is based on joint and, in most cases, simultaneous the work of the venous collectors of the gastrocnemius and soleus muscles, amazingly and harmoniously integrated into the general system of venous blood flow of the lower extremities.
The data we obtained about the features of the anatomical structure of the intramuscular veins of the leg using intravital visualization using MSCT venography can be used by ultrasound diagnostic specialists in describing the anatomical picture of venous hemodynamic disorders.
Expanding knowledge about the structural features of the veins of the gastrocnemius and soleus muscles and their topography will allow phlebologists to detail and more accurately interpret ultrasound duplex scanning data.
In addition, the information obtained will be the starting point in the research we have already begun on the influence of developing ectasia of the intramuscular veins of the leg on the formation and progression of chronic venous insufficiency of the lower extremities with various venous pathologies.
MSCT venography is the most informative method of intravital visualization of the venous system of the lower extremities, although it should be recognized that the method itself is invasive and expensive, and therefore cannot be widely used in everyday practice. However, the clarifications obtained and accumulated with its help about the structure of the venous collectors of the lower leg can help in constructing more accurate practical algorithms for solving diagnostic problems when using non-invasive methods for planning optimal treatment programs and predicting treatment results for patients with chronic venous insufficiency of the lower extremities caused by varicose veins or occlusive lesions.
Information about authors
Sannikov A.B. — Candidate of Medical Sciences, Associate Professor of the Department of Additional Professional Education of Health Care Specialists of the Russian National Research Medical University named after. N.I. Pirogov Ministry of Health of Russia, Moscow, Russia; https://orcid.org/0000-0003-1792-2434; e-mail
Emelyanenko V.M. - Doctor of Medical Sciences, Prof., Head. Department of Additional Professional Education of Health Care Specialists of the Russian National Research Medical University named after. N.I. Pirogov of the Russian Ministry of Health; https://orcid.org/0000-0003-0909-1693
Rachkov M.A. - head Department of Radiation Diagnostic Methods of the First Clinical Medical Center; https://orcid.org/0000-0002-7674-8221
Drozdova I.V. — doctor of functional diagnostics of the Medical University; https://orcid.org/0000-0002-2430-053Х
Author responsible
for correspondence:
Sannikov Alexander Borisovich - https://orcid.org/0000-0003-1792-2434; e-mail
How to quote:
Sannikov A.B., Emelyanenko V.M., Rachkov M.A., Drozdova I.V. Anatomical structure of the venous collector of the soleus muscle according to multislice computed tomography-venography. Operative surgery and clinical anatomy (Pirogov scientific journal).
2019;3(2):4-12. https://doi.org/10.17116/operhirurg201930214
Traditional methods
Alternative medicine also has an important place in the treatment of muscle pain. Common methods are foot baths with mint, linden flowers or lemon balm. They also prepare ointments and rub them into the sore spot at night.
- Mix egg yolk (1), turpentine (1 tsp), apple cider vinegar (1 tsp). Mix everything to a thick consistency. The ointment can be used immediately after preparation. Rub in overnight and wrap in a warm terry cloth.
- You can relieve muscle pain with cabbage leaves and soda. Grind the leaf in a meat grinder, add 2 tsp. soda, stir. The compress is applied 2 times a day for 20-30 minutes.
- Mix badger fat (1 tbsp), honey (1 tbsp) and turpentine (1 tsp). Everything is mixed and rubbed into painful muscles.
For burning in the soleus muscle, use a compress with water and alcohol in a 1:1 ratio. The bandage is applied for 30 minutes, 2 times a day.
Pepper tincture has a warming effect, which is also used to warm the soleus muscle. An infusion kit can be purchased at a pharmacy or made independently at home.
To do this you will need:
- crushed red chili pepper (2 pcs.);
- honey (2 tbsp);
- moonshine (250 ml);
- celery, dill and caraway seeds are used in dry form, 2 tbsp each. l.
Everything is mixed and infused for 5 days in a dark, cool place. Then shake and strain. Use as a lotion for 15 minutes, morning and evening.
A medicinal bath with the addition of pine needles and chamomile is used. Medicinal plants are valuable for their oils, vitamins and amino acids. They relieve inflammation and normalize blood supply to tissues, relieve fatigue, tension and provide muscle tone.
Epsom salt baths will help regulate nerve signals in the body, as the salt acts as a natural muscle relaxant. Thanks to salt, pain is reduced and swelling is relieved. Add 1/2 tbsp to warm water. salt and lower your feet for 15-20 minutes.
Horse chestnut is often used in natural remedies for vein diseases, as it provides relief and preventive action. Rock clover is another effective remedy.
The herb has an antithrombotic effect, promotes blood circulation and has a decongestant effect - all of which benefit the veins. Comfrey has similar properties and is used in both ointments and tea. However, it should be noted that effective herbs are not suitable for long-term therapy.
Sciatic nerve neuropathy. Piriformis syndrome
Diseases of the peripheral nervous system are one of the most common causes of disability in patients of working age. In the structure of these diseases, pain syndromes occupy a predominant place (N. N. Yakhno, 2003; G. R. Tabeeva, 2004). The reasons for the development of neuropathic pain syndrome can be different: diabetes mellitus, paraneoplastic processes, HIV, herpes, chronic alcoholism (A. M. Vein, 1997; I. A. Strokov, A. N. Barinov, 2002).
When the peripheral nervous system is damaged, two types of pain are distinguished: dysesthesia and truncal. Superficial dysesthetic pain is usually observed in patients with predominant damage to small nerve fibers. Truncal pain occurs with compression of the spinal roots and tunnel neuropathies.
In patients with this type of pain syndrome, it is impossible to choose the optimal treatment strategy without identifying the pathophysiological mechanisms. Therefore, when determining treatment tactics, it is necessary to take into account the localization, nature and severity of clinical manifestations of pain.
Compression-ischemic (tunnel) neuropathy refers to non-inflammatory lesions of the peripheral nerve that develop under the influence of compression or ischemic influences.
In the area of compression of the corresponding nerve, painful compactions or thickening of tissue are often found, leading to a significant narrowing of the musculoskeletal sheaths through which the neurovascular trunks pass.
Currently, many variants of compression neuropathies are known. Their clinical picture consists of three syndromes: vertebral (in cases where the factor of the same name is involved), neural peripheral, reflex-myotonic or dystrophic. Vertebral syndrome at any stage of exacerbation, and even in remission, can cause changes in the walls of the “tunnel”. The myodystrophic focus, acting as a implementing link, causes neuropathy against the background of its clinical peak. The neurological picture of compression neuropathies consists of symptoms of damage of varying severity in the corresponding myo- and dermatomes. The diagnosis of compression neuropathies is made in the presence of pain and paresthesia in the area of innervation of this nerve, motor and sensory disorders, as well as pain in the area of the receptors of the corresponding channel and Tinel’s vibration symptom. If there are difficulties in diagnosis, electroneuromyographic studies are used: lesions of the peripheral neuron corresponding to a given nerve are determined, and the degree of decrease in the speed of impulse transmission along the nerve distal to the place of its compression. Piriformis syndrome is the most common tunnel neuropathy. Pathological tension of the piriformis muscle due to compression of the L5 or S1 root, as well as with unsuccessful injections of medicinal substances, leads to compression of the sciatic nerve (or its branches at high origin) and the accompanying vessels in the infrapiriformis space.
To choose the right treatment strategy, it is necessary to clearly know the main clinical symptoms of damage to a particular area. The main clinical manifestations of damage to the nerves of the sacral plexus:
- compression of nerves in the pelvis or above the gluteal fold;
- piriformis syndrome;
- damage to the sciatic nerve below the exit from the pelvis (at the level of the hip and below) or damage to the sciatic nerve in the pelvic cavity;
- sciatic nerve syndrome;
- tibial nerve syndrome;
- syndrome of the piriformis, internal obturator nerves and quadratus femoris nerve;
- superior gluteal nerve syndrome;
- inferior gluteal nerve syndrome.
The most difficult in terms of diagnosis are lesions in the pelvic area or above the gluteal fold - due to the presence of somatic or gynecological pathology in patients. Clinical symptoms of lesions in the pelvis or above the gluteal fold consist of the following types of disturbances of motor and sensory functions.
- Decrease and loss of function n. peroneus and n. tibialis communis, paralysis of the foot and fingers, loss of the Achilles and plantar reflexes, hypoesthesia (anesthesia) of the leg and foot.
- Reduction or loss of function of the biceps femoris, semimembranosus and semitendinosus muscles, leading to impaired flexion of the leg.
- Reduction or loss of function of the posterior cutaneous nerve of the thigh, leading to hypoesthesia (anesthesia) along the posterior surface of the thigh.
- Difficulty in external rotation of the hip.
- Presence of positive symptoms in Lasegue, Bonnet.
- The presence of vasomotor and trophic disorders (hypo-, hyperhidrosis, formation of trophic ulcers in the heel and outer edge of the foot, changes in nail growth, hypo- and hypertrichosis).
Damage to the sciatic nerve at the level of the infrapiriform foramen can be observed in two variants:
- damage to the trunk of the sciatic nerve itself;
- piriformis syndrome.
Compression of the sciatic nerve and adjacent vessels is characterized by the following clinical manifestations: a feeling of constant heaviness in the leg, dull, “cerebral” pain. There is no increase in pain when coughing or sneezing. There is no atrophy of the gluteal muscles. The zone of hypoesthesia does not extend above the knee joint.
Piriformis syndrome occurs in at least 50% of patients with discogenic lumbosacral radiculitis. If the patient is diagnosed with this, the assumption of the presence of piriformis muscle syndrome may arise in the presence of persistent pain along the sciatic nerve that does not decrease with drug treatment. It is much more difficult to determine the presence of this syndrome if there is only pain in the buttock area, which is limited in nature and associated with certain positions (movements) of the pelvis or when walking. Piriformis muscle syndrome is often recorded in gynecological practice. With piriformis syndrome it is possible:
- compression of the sciatic nerve between the altered piriformis muscle and the sacrospinous ligament;
- compression of the sciatic nerve by the altered piriformis muscle as the nerve passes through the muscle itself (a variant of the development of the sciatic nerve).
The clinical picture of piriformis syndrome consists of local symptoms and symptoms of compression of the sciatic nerve. Local includes aching, nagging, “braining” pain in the buttock, sacroiliac and hip joints, which intensifies when walking, standing, adducting the hip, and also in a squatting position; subsides somewhat when lying down and sitting with legs apart. With good relaxation of the gluteus maximus muscle, a dense and painful when stretched (Bonnet-Bobrovnikova symptom) piriformis muscle is felt underneath it. With percussion at the point of the piriformis muscle, pain appears on the back of the leg (Vilenkin's symptom). The clinical picture of compression of the vessels and the sciatic nerve in the infrapiriform space consists of the topographic-anatomical “relationship” of its tibial and fibular branches with the surrounding structures. Pain during compression of the sciatic nerve is dull, “brainy” in nature with a pronounced vegetative coloring (sensations of chilliness, burning, stiffness), with irradiation throughout the leg or mainly along the zone of innervation of the tibial and peroneal nerves. Provoking factors are heat, weather changes, and stressful situations. Sometimes the Achilles reflex and superficial sensitivity decrease. With the predominant involvement of the fibers from which the tibial nerve is formed, the pain is localized in the posterior group of muscles of the leg. Pain appears in them when walking, during the Lasègue test. Palpation reveals pain in the soleus and gastrocnemius muscles. In some patients, compression of the inferior gluteal artery and the vessels of the sciatic nerve itself is accompanied by a sharp transient spasm of the vessels of the leg, leading to intermittent claudication. The patient is forced to stop, sit down or lie down when walking. The skin of the leg turns pale. After resting, the patient can continue walking, but soon the same attack recurs. Thus, in addition to intermittent claudication with obliterating endarteritis, there is also infrapiriform intermittent claudication. An important diagnostic test is infiltration of the piriformis muscle with novocaine and assessment of the positive changes that occur. Reflex tension in the muscle and neurotrophic processes in it are caused, as a rule, by irritation not of the fifth lumbar, but of the first sacral root. Certain manual tests help recognize this syndrome.
- The presence of pain on palpation of the upper internal region of the greater trochanter of the femur (the place of attachment of the piriformis muscle).
- Pain on palpation of the lower part of the sacroiliac joint is a projection of the attachment site of the piriformis muscle.
- Passive adduction of the hip with simultaneous internal rotation (Bonnet-Bobrovnikova symptom; Bonnet symptom).
- A test to examine the sacrospinous ligament, which allows you to simultaneously diagnose the condition of the sacrospinous and iliosacral ligaments.
- Tapping the buttock (on the sore side). This causes pain that spreads along the back of the thigh.
- Grossman's sign. When struck with a hammer or folded fingers on the lower lumbar or upper sacral spinous processes, the gluteal muscles contract.
Since painful tension of the piriformis muscle is most often associated with irritation of the first sacral root, it is advisable to alternately carry out novocaine blockade of this root and novocainization of the piriformis muscle. A significant reduction or disappearance of pain along the sciatic nerve can be considered a dynamic test showing that the pain is caused by the compressive effect of the spasmed muscle.
Sciatic nerve lesions
Lesions of the sciatic nerve below the exit from the pelvis (at the level of the hip and below) or in the pelvic cavity are characterized by the following signs.
- Impaired flexion of the leg at the knee joint (paresis of the semitendinosus, semimembranosus and biceps femoris muscles).
- Specific gait: the straightened leg is carried forward when walking (due to the predominance of the tone of the antagonist muscle of the quadriceps femoris).
- Straightening the leg at the knee joint is a contraction of the antagonist (quadriceps femoris muscle).
- Lack of active movements in the foot and fingers as a result of their paresis.
- Atrophy of paralyzed muscles, which often masks the pastiness of the limb.
- Hypoesthesia along the posterior surface of the leg, dorsum of the foot, sole and toes.
- Impaired muscle-articular sensitivity in the ankle joint and interphalangeal joints of the toes.
- Lack of vibration sensitivity in the area of the outer ankle.
- Pain along the sciatic nerve - at the Valle and Gar points.
- Positive Lasegue symptom.
- Reduction or disappearance of the Achilles and plantar reflexes.
- The presence of burning pain that intensifies when lowering the leg.
In addition to the clinical symptoms described above, the development of vasomotor and trophic disorders is likely: increased skin temperature on the affected leg. The lower leg and foot become cold and cyanotic. Hyperhidrosis or anhidrosis, hypotrichosis, and hyperkeratosis are often found on the sole. Changes in the color and shape of the nails, trophic disorders on the heel, dorsum of the toes, and the outer edge of the foot appear, a decrease in strength is recorded, as well as atrophy of the muscles of the foot and lower leg. The patient cannot stand on his toes or heels. The semitendinosus, semimembranosus, and biceps femoris strength tests can be used to determine initial sciatic nerve involvement.
Sciatic nerve syndrome (ischemic-compressive neuropathy of the sciatic nerve). Depending on the level (height) of the lesion, different variants of sciatic nerve syndrome are possible.
A very high level of damage (in the pelvis or above the gluteal fold) is characterized by: paralysis of the foot and toes, loss of the Achilles and plantar reflexes; anesthesia (hypoesthesia) of almost the entire lower leg and foot, except for zone n. sapheni; loss of function of the biceps femoris, semitendinosus, semimembranosus muscles; hypoesthesia (anesthesia) along the posterior surface of the thigh; inability to rotate the hip outward; the presence of positive symptoms of tension (Lasegue, Bonnet); the presence of vasomotor and trophic disorders (hyper- or hypotrichosis, hypo- or hyperhidrosis, changes in nail growth, the formation of trophic ulcers in the heel area and the outer edge of the foot).
A lesion at the level of the infrapiriformis foramen consists of two groups of symptoms - damage to the piriformis muscle itself and the sciatic nerve. The first group of symptoms includes: pain on palpation of the upper internal part of the greater trochanter of the femur (the place of attachment of the piriformis muscle to the capsule of this joint); pain on palpation in the lower part of the sacroiliac joint; Bonnet's symptom (passive adduction of the hip with its inward rotation, causing pain in the gluteal region, less often in the zone of innervation of the sciatic nerve); pain on palpation of the buttock at the point where the sciatic nerve exits from under the piriformis muscle. The second group includes symptoms of compression of the sciatic nerve and blood vessels. Painful sensations due to compression of the sciatic nerve are characterized by a feeling of constant heaviness in the leg, a dull, “cerebral” nature of the pain, no increase in pain when coughing and sneezing, as well as atrophy of the gluteal muscles; the hypoesthesia zone does not rise above the knee joint.
A lesion at the level of the hip (below the exit from the pelvis) and up to the level of division into the peroneal and tibial nerves is characterized by: impaired flexion of the leg at the knee joint; specific gait; lack of active movements in the foot and toes, which sag moderately; atrophy of paralyzed muscles that joins after 2–3 weeks, often masking the pastiness of the leg; hypoesthesia (anesthesia) on the posterior surface of the leg, dorsum of the foot, sole and toes; impairment of joint-muscular sensitivity in the ankle joint and interphalangeal joints of the toes; lack of vibration sensitivity on the outer ankle; pain along the sciatic nerve - at the points of Valle and Gar; positive Lasegue symptom; disappearance of the Achilles and plantar reflexes.
The syndrome of incomplete damage to the sciatic nerve is characterized by the presence of pain of a causalgic nature (“burning” pain, intensified when lowering the leg, provoked by a light touch); severe vasomotor and trophic disorders (for the first 2–3 weeks, the skin temperature on the affected leg is 3–5 °C higher (“hot skin”) than on the healthy leg, then the lower leg and foot become cold and cyanotic). Hyperhidrosis or anhidrosis, hypotrichosis, hyperkeratosis, changes in the shape, color and growth rate of nails are often found on the plantar surface. Sometimes trophic ulcers occur on the heel, the outer edge of the foot, and the dorsum of the toes. X-rays reveal osteoporosis and decalcification of the foot bones.
Initial sciatic nerve injury syndrome can be diagnosed by using tests to determine the strength of the semitendinosus and semimembranosus muscles.
Sciatic nerve syndrome most often appears as a result of damage to this nerve through the mechanism of tunnel syndrome when the piriformis muscle is involved in the pathological process. The trunk of the sciatic nerve can be affected by injuries, fractures of the pelvic bones, inflammatory and oncological diseases of the pelvis, lesions and diseases of the gluteal region, sacroiliac joint and hip joint. In sciatic nerve syndrome, the differential diagnosis often has to be made with discogenic compressive radiculitis LV-SII (Table).
Syndrome of the piriformis, internal obturator and quadratus femoris nerves. Complete piriformis, obturator internus, and quadratus femoris nerve syndrome is characterized by impaired lateral rotation of the hip. The syndrome of partial damage to this group of nerves can be diagnosed based on the use of tests to determine the range of motion and strength of the subject.
Superior gluteal nerve syndrome. Complete superior gluteal nerve syndrome is characterized by impaired abduction of the hip with partial impairment of hip rotation and difficulty maintaining an upright position of the torso. With bilateral paralysis of these muscles, it is difficult for the patient to stand (stands unsteadily) and walk (the so-called “duck walk” appears with waddling from side to side). Partial superior gluteal nerve syndrome can be identified with a gluteal strength test. Based on the degree of decrease in strength compared to the healthy side, a conclusion is made about partial damage to the superior gluteal nerve.
Inferior gluteal nerve syndrome. Complete inferior gluteal nerve syndrome is characterized by difficulty in straightening the leg at the hip joint, and in a standing position - difficulty in straightening a tilted pelvis (the pelvis is tilted forward, with compensatory lordosis observed in the lumbar spine). Difficulty getting up from a sitting position, climbing stairs, running, jumping. With prolonged damage to this nerve, hypotonia and hypotrophy of the gluteal muscles are observed. Partial inferior gluteal nerve syndrome can be diagnosed using a test to determine the strength of the gluteus maximus muscle. Based on the degree of decrease in the volume and strength of the indicated movement (and in comparison with the healthy side), a conclusion is made about the degree of dysfunction of the inferior gluteal nerve.
Treatment
Therapy of sciatic nerve neuropathy requires knowledge of the etiological and pathogenetic mechanisms of the development of the disease. Treatment tactics depend on the severity and rate of progression of the disease. Pathogenetic therapy should be aimed at eliminating the pathological process and its long-term consequences. In other cases, treatment should be symptomatic. Its goal is to prolong stable remission and improve the quality of life of patients. The main criterion for the optimal therapeutic effect on the patient is the combination of medicinal and non-medicinal methods. Among the latter, the leading ones are physiotherapeutic techniques and post-isometric relaxation methods.
If the function of the muscles of the pelvic girdle and lower limb is impaired, it is recommended to use one of the manual therapy techniques - post-isometric relaxation (PIR), i.e. stretching the spasmodic muscle to its physiological length after maximum tension. The basic principles of drug therapy for lesions of the peripheral nervous system are early initiation of treatment, pain relief, and a combination of pathogenetic and symptomatic therapy. Pathogenetic therapy is aimed primarily at combating oxidative stress, affecting the microvasculature, improving blood supply to the affected area, and relieving signs of neurogenic inflammation. For this purpose, antioxidant, vasoactive and nonsteroidal anti-inflammatory drugs (NSAIDs) are used. The complexity of drug therapy is associated in most cases with the intricate anatomical and physiological hierarchy of structures involved in the pathological process. This is partly due to the structure and functioning of the structures of the lumbosacral plexus. At the same time, the basic mechanism underlying the development of neuropathy is a clear correlation between compression and ischemia of the nerve and the development of oxidative stress.
Oxidative stress is an imbalance between the production of free radicals and the activity of antioxidant systems. The developed imbalance leads to increased production of compounds (neurotransmitters) released by damaged tissues: histamine, serotonin, ATP, leukotrienes, interleukins, prostaglandins, nitric oxide, etc. They lead to the development of neurogenic inflammation, increasing the permeability of the vascular wall, and also promote the release mast cells and leukocytes of prostaglandin E2, cytokines and biogenic amines, increasing the excitability of nociceptors.
Currently, clinical studies have appeared on the use of drugs that improve the rheological properties of blood and endothelium-dependent reactions of the vessel wall in patients with compression neuropathies. Drugs such as thioctic acid derivatives (thiogamma, thioctacid) and ginkgo biloba (tanakan) are successfully used to reduce the manifestations of oxidative stress. However, the use of drugs with a polyvalent mechanism of action (Cerebrolysin, Actovegin) is more pathogenetically justified.
The priority of using Actovegin is due to the possibility of its use for therapeutic blockades and its good compatibility with other drugs. For compression-ischemic neuropathies, both in the acute and subacute stages of the disease, it is advisable to use Actovegin, especially if there is no effect from other treatment methods. A drip of 200 mg of the drug is prescribed for 5 days, followed by a transition to oral administration.
In the mechanisms of development of diseases of the peripheral nervous system, an important place is occupied by hemodynamic disorders in the structures of the peripheral nervous system, ischemia, microcirculation disorders, energy exchange disorders in ischemic neurons with a decrease in aerobic energy exchange, ATP metabolism, oxygen and glucose utilization. Pathological processes occurring in nerve fibers during neuropathies require correction with vasoactive drugs. In order to improve microcirculation processes and activate metabolic and glycolysis processes in patients with tunnel neuropathies, Cavinton, Halidor, Trental, and Instenon are used.
Instenon is a combined drug with neuroprotective action, including a vasoactive agent from the group of purine derivatives, affecting the state of the ascending reticular formation and cortical-subcortical relationships, as well as the processes of tissue respiration under hypoxic conditions, physiological mechanisms of autoregulation of cerebral and systemic blood flow. For neuropathies, instenon is used intravenously, 2 ml in 200 ml of saline, for 2 hours, 5–10 procedures per course. Then oral administration of instenon forte continues, 1 tablet 3 times a day for a month. For neuropathies with sympathetic syndrome, the use of instenon 2 ml intramuscularly once a day for 10 days is indicated. For compression-ischemic (tunnel) neuropathies, a similar technique is used. This helps improve microcirculation and metabolism in the ischemic nerve. A particularly good effect is observed with the combined use of Actovegin (drops) and instenon (intramuscular injections or oral administration).
Halidor (bencyclane fumarate) is a drug with a wide spectrum of action, which is due to the blockade of phosphodiesterase, antiserotonin effect, and calcium antagonism. Halidor is prescribed in a daily dose of 400 mg for 10–14 days.
Trental (pentoxifylline) is used 400 mg 2-3 times a day orally or 100-300 mg intravenously in 250 ml of saline.
Prescribing combination drugs that include large doses of vitamin B, anti-inflammatory drugs and hormones is inappropriate.
NSAIDs remain the first-line drugs for pain relief. The main mechanism of action of NSAIDs is inhibition of cyclooxygenase (COX-1, COX-2), a key enzyme in the arachidonic acid metabolic cascade, leading to the synthesis of prostaglandins, prostacyclins and thromboxanes. Due to the fact that COX metabolism plays a major role in the induction of pain at the site of inflammation and the transmission of nociceptive impulses to the spinal cord, NSAIDs are widely used in neurological practice. There is evidence that 300 million patients take them (G. Ya. Schwartz, 2002).
All anti-inflammatory drugs have anti-inflammatory, analgesic and antipyretic effects, are able to inhibit the migration of neutrophils to the site of inflammation and platelet aggregation, and also actively bind to serum proteins. Differences in the action of NSAIDs are quantitative (G. Ya. Schwartz, 2002), but they determine the severity of the therapeutic effect, tolerability and the likelihood of side effects in patients. The high gastrotoxicity of NSAIDs, which correlates with the severity of their sanogenetic effect, is associated with indiscriminate inhibition of both isoforms of cyclooxygenase. In this regard, for the treatment of severe pain syndromes, including long-term ones, drugs are needed that have anti-inflammatory and analgesic effects with minimal gastrotoxic reactions. The most well-known and effective drug from this group is xefocam (lornoxicam).
Xefocam is a drug with a pronounced antianginal effect, which is achieved through a combination of anti-inflammatory and strong analgesic effects. It is today one of the most effective and safe modern analgesics, which has been confirmed by clinical studies. The effectiveness of oral administration according to the following regimen: 1st day - 16 and 8 mg; Days 2–4 - 8 mg 2 times a day, day 5 - 8 mg/day - for acute back pain has been reliably proven. The analgesic effect at a dose of 2–16 mg 2 times a day is several times higher than that of napraxen. For tunnel neuropathies, it is recommended to use the drug in a dose of 16–32 mg. The course of treatment is at least 5 days with a one-time daily procedure. It is recommended to use the drug Xefocam for the treatment of piriformis muscle syndrome according to the following method: in the morning - 8 mg intramuscularly, in the evening - 8-16 mg orally, for 5-10 days, which allows you to achieve a quick and accurate effect on the source of inflammation with complete anesthesia with minimal risk development of adverse reactions. It is possible to carry out regional intramuscular blockades in the paravertebral region, 8 mg per 4 ml of 5% glucose solution daily for 3–8 days. Symptomatic therapy is the method of choice for relieving algic manifestations. Most often, therapeutic blockades with anesthetics are used to treat tunnel neuropathies. Persistent pain lasting more than 3 weeks indicates a chronic process. Chronic pain is a complex therapeutic problem that requires an individual approach.
First of all, it is necessary to exclude other causes of pain, after which it is advisable to prescribe antidepressants.
M. V. Putilina , Doctor of Medical Sciences, Professor of Russian State Medical University, Moscow
Other methods
The soleus muscle is in contractile processes from time to time. This reaction is accompanied by pain and swelling. Norepinephrine is released and a neuromuscular enzyme is formed. The specialist will determine the treatment method based on the type of disease.
- Massage. It is carried out only by a specialist who will relieve overvoltage. Give a massage after removing foci of inflammation. Home massage is not helpful in this matter, as it will only alleviate the symptoms.
- Physiotherapeutic activities . This method treats myalgia. Electrophoresis is used in a composition with calcium chloride. Exceptions include electrical muscle stimulation and thermal treatment.
- Gymnastic exercises. Improves muscle condition during stationary work. Physical exercises are prescribed by a specialist.
- Manual therapy. The most effective method of muscle treatment, common in China.
By using friction therapy, the healing process of the soleus muscle is accelerated. The patient lies face down on a special table in the massage room. The massage therapist bends the leg 90 degrees. After this, the massage therapist's ankle is placed on the patient's shoulder, but the knee must be bent.
Next, grab the leg with your hands, and your fingertips should look at the calf. The shin is held with the thumb. Then the massage therapist grasps the patient’s leg bent at the knee to perform smooth circular movements of the leg in a bent position. Treatment with such procedures lasts 15-20 minutes.
Kinesiotherapy is another effective method for treating chronic muscle inflammation and injury. Limits the load on the injured area, heals and restores the cellular structure of muscle fibers.
The tape is applied in the direction of the fibers of all the soleus muscles, since it is located topographically under the gastrocnemius muscle, and therefore taping it is sometimes impossible.
Shock wave complex therapy is also used. Thanks to a special drug, the therapy generates an infrasonic wave. The waves penetrate the affected tissues, and increase blood flow, relieve swelling and inflammation.
Usually 5-7 sessions are enough, one of which lasts no more than 15 minutes. Contraindications to such therapy are: tumor, pregnancy. After the procedure, the pain usually stops.
During the first stage of pain, the patient requires rest. Apply ice to the sore spot for 15 minutes, every hour, wrap it in a towel, to prevent internal bleeding.
Lie down on the bed and raise your legs, placing them on the pillows. Moderate injuries can be treated well with stretching exercises that improve blood circulation to the muscle.
The doctor may prescribe muscle relaxants that relieve muscle spasms and B vitamins that strengthen the nerves. Athletes often use manual therapy, which completely relieves muscle pain, tightness and contraction.
Exercises for the calf muscles
We already know that the calf muscles are most active when a person is in a standing position and his legs are straight. This leads to the main condition for training the calf muscles – straight legs in a standing position.
Standing calf raises
The most popular and, so to speak, basic calf exercise is standing calf raises . For this exercise, both a special machine and a Smith machine are suitable.
You can use a sock holder or not, but I recommend using it. The height of the stand should be such that at the lowest point the heels never touch the floor. It is not necessary to specifically go as low as possible; a slight stretch at the bottom point is quite enough. The stand allows you to increase the range of motion, which is very small in lower leg exercises.
The legs at the knee joint can be either absolutely straight or slightly bent. You should keep your back straight; you should not push your pelvis too far back. In general, the bar on your shoulders should be in line with your toes.
Standing calf raises can also be done with dumbbells. In this embodiment, you need to hold onto a support with one hand to maintain balance, and hold a dumbbell in the other. Each shin is worked alternately.
Bent-over calf raises (“donkey”)
An interesting and effective exercise is standing calf raises or the so-called “donkey”. To perform this exercise, you need to tilt your body forward, leaving your legs straight. A significant disadvantage of this exercise is that the load on the calves is not great enough and there is nothing left to do but put a partner on your back and lift with him. But even with a partner, the load may not be enough. Therefore, a great substitute for this exercise would be the toe press on a leg press machine. The advantages are obvious - there is no load on the back and wide adjustment of the degree of load. Such machines are available in almost every fitness club.
Possible complications
To prevent muscle rupture, it is necessary to constantly warm them up before training. The most dangerous thing about a muscle rupture is that without the correct medical assistance from a surgeon, the soleus muscle may not heal properly and be in a displaced location.
Chronic defects also form that cannot be eliminated or cured, even with the help of a surgeon. Therefore, after undergoing muscle diagnostics and treatment, you can promptly restore the vital activity of the soleus muscle in order to enjoy training again.
If you experience severe pain, you should definitely consult a doctor. Thanks to complex treatment, which is at the stage of drug therapy, therapeutic exercises and massage, the soleus muscle will recover in the shortest possible time and without complications.
Interesting trick
There is another interesting training technique that will help you “break through” a stubborn shin. This is a rest-pause. Personally, I use this technique as the last set of the calf exercise. After completing 4 sets of 10 reps, I step off the stand, rest for 15 seconds, then get back on the stand and do a few reps, usually about seven. Then I rest again for 15 seconds and repeat everything again until the number of repetitions drops to three. Since the lower leg is a very durable muscle group, the number of such approaches will be quite large. I need 6-7 sets to get the number of reps down from seven to three. After such an execution, the shin feels pleasantly sore for several days.